We may have learnt to tame it with drugs, but pain is one of the certainties of human existence. It can be both physical and emotional, ranging from a searing torment to a mild soreness.
But what exactly is pain? What function does it serve, and how can we really know how much pain someone is in?
What is pain?
Simple, you’d think. You touch a hot saucepan by mistake and it hurts like hell. You immediately withdraw your hand, rush to the tap and run cold water over it. Phew. No need to rush to A&E.
But then it throbs for days, reminding you of the burn and your carelessness until the pain fades away. Lesson learned: you’ll be more careful around cookers in future.
This simple incident can tell us a lot about pain. Mostly, it’s a brilliant warning system.
Read more about pain:
- Could painkillers also kill pleasure?
- The cause of migraines could be in sight (literally)
- Women might not remember pain as much as men
Without it, you would not have withdrawn your hand, and the injury would be much worse. Pain like this – what we call ‘acute pain’ – is a good thing: it’s key to our survival. That’s why the ability to experience pain is shared across species.
A few people include plants in this, too, but as plants have no nervous system or brain, it’s hard to know how they’d actually feel pain when injured or cut. Pain is evolutionarily old, an essential warning that something in the environment can cause us injury, harm, or even death.

Without pain, you’re in trouble. We know this, sadly, because there’s a rare genetic condition, which we call ‘congenital insensitivity to pain’ or CIP, in which a person doesn’t get the warning ‘hurt’ of pain after severely damaging themselves.
Historically, they didn’t survive to adulthood due to the consequences of unfelt injury.
What does pain do?
Pain motivates us to act. Think about that hot pan again. Now imagine you’d picked up the pan before realising it was too hot to handle. Your options are to drop it and make a mess, or bear the pain until a solution is found.
In an instant, you detect that the pan is hot (thermal), it’s on your hand (location), it’s painful (intensity), you don’t like it (unpleasant), it’s engaged your full attention (cognition), and you’re not happy about it (emotional). That’s a lot of things, which is why pain is often called a ‘multidimensional’ experience.
So, what do you do? Well, from past experiences, learnt responses, and potential outcomes (like being told off for dropping the pan) you make a decision and act. Recruiting extraordinary brain-based networks, you are able to block the pain and get the hot pan to safety – then it’s back to that cold tap.
Pain drives action, prompting us to run away, avoid it in the first place, or signal to others that we need help and relief.
How do we feel pain?
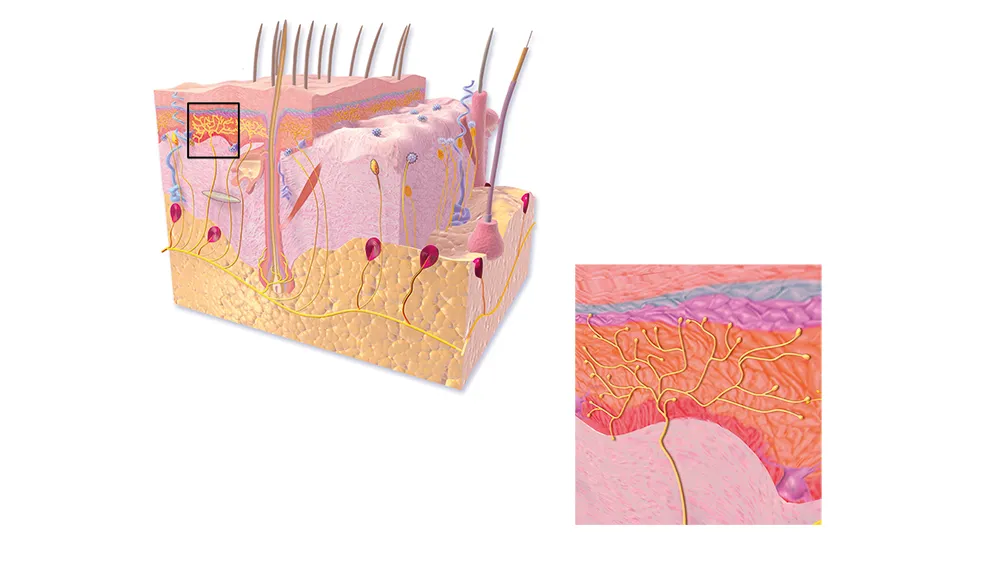
Just underneath our skin surface, we have an intricate network of ‘pain nerve fibres’ that end with special receptors called nociceptors. When activated, these receptors send signals along the nerve fibres to the spinal cord and up into the brain, where pain, as a perception, emerges.
The nociceptors can be activated by a variety of triggers: thermal (heat), mechanical (like a knife cut or hammer blow) and chemical/irritant (for example, acid or chilli pepper).
The signals then travel along different types of pain nerve fibre. A∂, also known as A-delta, fibres carry what we call ‘first pain’ – the fast, quick signal that tells you ‘ouch’ when you touch a hot pan.
C fibres follow up with the ‘second pain’, which is the slow, constant throbbing that tells you it’s still hurting. Normal touch – feeling something like your clothes or holding a pen – is carried on different peripheral nerves called Aß (A-beta).
The transmission of the pain signal to the spinal cord is helped by other components of the nerve fibres called ion channels, and it’s these that many patients with CIP don’t have, which is why they don’t feel pain.
Therefore, targeting and blocking nociceptors and/or the transmission process is a cunning way to block pain. Indeed, that’s what many pharmaceutical companies are currently trying to do.
Interestingly, many nociceptors are ‘polymodal’ – a fancy word meaning that different things can activate the same nociceptor.
As an example, let’s look at temperature and food.
How can food be painful?
Different thermal nociceptors in our body are activated by specific temperatures, giving us a painful sensation of intense hot or cold.
Amazingly, these same nociceptors are also activated by various natural chemicals, giving rise to the same experience. For instance, when we bite into a chilli pepper, a chemical called capsaicin binds to the same nociceptor that’s activated by painfully hot temperatures of around 42°C and above.
That’s why we perceive a curry as hot: the brain can’t distinguish what activated the nociceptor, it just knows that your mouth is burning! Downing a pint of lager won’t help, either, as capsaicin is fat-soluble, not water-soluble – so order a cucumber raita instead.

Some scientists think that plants produce capsaicin to discourage mammals from eating their fruits.
Birds don’t seem to react to the chemical, allowing them to eat the chillies and help with seed dispersal and plant reproduction – which is what the plant wants!
How does the brain generate pain?
Once the pain signals arrive from the spinal cord to the brain, a large network of brain regions is activated, including the brainstem, the thalamus and several regions of the cortex. The subjective experience of pain then emerges from this brain activity.
Until the conscious brain processes these incoming signals, we don’t actually call it pain, but nociception – this is the nervous system’s response to the original tissue damage. The relationship between the extent of tissue damage and the amount or quality of pain that the person actually feels is not a simple one-to-one mapping.
Incoming signals can be amplified, attenuated or reappraised by the brain, which can dramatically change the individual’s experience. So, being sad about your pain or being anxious at the dentist really will make it worse – emotions are like amplifiers in your brain, turning up the volume of pain.
Thankfully, we also have an inbuilt system to lessen pain. The brain system that’s responsible for the feelings of pain can talk to the spinal cord and suppress nociceptive signals, like a brake.
This results in less brain activity and less pain, at least until the brake is removed. This is what goes on in athletes and soldiers during situations of high arousal and battle, or when someone is distracted from their pain (for example, a parent desperately distracting their child from the dreaded vaccine jab).

It’s not a trick, but real physiology. In fact, it’s this system, called the ‘descending pain modulatory system’, that’s hijacked when the placebo effect acts to reduce pain. This is known as ‘placebo analgesia’.
Weirdly, it was once thought, not too long ago, that because animals and babies have less developed brains than adults, they cannot feel pain. This is complete nonsense.
Pain is an individualised and subjective experience that depends upon a person’s mood, how much attention they give to it, the context of the situation in which they are hurt and so on – and it doesn’t need a fully-developed brain to take place.
What is the difference between physical and emotional pain?
Historically, if people reported pain in the absence of an injury, it was called ‘psychogenic’ pain – a pejorative term due to a flawed understanding of the mechanisms involved.

Emotional pain also has a neural basis, and there are even overlaps with some brain regions involved in physical pain. Understanding the basis of someone’s pain is important if we’re going to help them.
For example, is the pain due to inputs from the body, or has the brain generated an experience independently? We shouldn’t think that physical pain is more ‘real’ or important than emotional pain.
What is chronic pain?
This is the system gone wrong. It’s defined as pain that persists beyond normal tissue healing time. A staggering one in five adults experiences it. It lasts, on average, for seven years, but for 20 per cent of people it’s more than 20 years, and is more prevalent in women and the elderly. Chronic pain wreaks suffering on patients and their families.
It also brings significant costs to society, estimated annually at €200bn in Europe and $600bn in the US. Additional problems like depression, anxiety and sleeplessness can add to the suffering.
Chronic pain is one of the largest health problems worldwide, and current treatment options do not provide adequate relief to the majority of patients. Patients with chronic pain might have different conditions. Nerve damage due to diabetes, being on chemotherapy, multiple sclerosis, sustaining an injury, phantom limb pain, or arthritis, are a few examples.
Yet the signs and symptoms that patients describe are often similar. We are starting to consider chronic pain as a disease in its own right, with underpinning problems that we can work on and try to fix.
A key problem in chronic pain is that A∂ and C fibres can switch on permanently when damaged, sending constant pain signals to the sufferer’s brain. Second, it’s been shown that the pathway from nociceptor to brain can get ‘sensitised’ so that the signals are amplified. This makes the situation worse, causing even the touch of clothing or bedsheets to become painful.
Imagine that, but worse, going on for years alongside additional constant pain.
How can we know how much pain someone is in?

It’s important to signal when we’re in pain because this drives empathy and compassion in others, as well as eliciting help. Generally, we use behavioural observations and language to work out if someone is suffering.
People grimace, writhe or cry out in agony. But it’s hard to measure pain, as it’s such a subjective experience.
If language is available, then rating scales can help to capture features of the pain such as intensity and unpleasantness (0 = no pain, 10 = excruciating). But I doubt your 10 is my 10.
Questionnaires can be used instead of number scales, and sometimes just smiley or sad faces, such as with children. Pain levels of babies, comatose or anaesthetised individuals, or dementia patients may be more difficult to judge, and it’s tough to know what they’re really feeling.
Read more about the brain and pain:
- If the brain has no pain receptors, why do I get headaches?
- Could pain be the other side of happiness?
Looking at body measures, like heart or breathing rate, can help. Some studies suggest that women are more sensitive to pain than men, but perhaps women cope better – we all know about man flu! Brain imaging is helping us to understand pain better, but it should not be used as a surrogate for what the person reports.
The International Association for the Study of Pain defines pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”. In short, if the person says they are in pain, then they are – no matter what caused it.
How do we treat pain?
Painkillers provide relief from pain. The two oldest are aspirin, which is derived from willow bark, and morphine, which comes from opium poppies. These days, aspirin is largely replaced by ibuprofen if there is inflammation, or paracetamol if there is no inflammation.
Morphine is an opioid and variants of it are still widely used, but can have associated problems like tolerance and addiction. Other painkillers include different types of anti-inflammatory style drugs, antidepressants, and anticonvulsants.

There are many additional treatments for pain, including cognitive behavioural therapy, physiotherapy and surgery, and the most effective therapies combine all of these treatments.
With new drugs coming through the pipeline, and our understanding of pain constantly improving, we can hope for a future where no one will have to suffer unnecessary pain.
- This article first appeared in issue 311 of BBC Focus Magazine–find out how to subscribe here
JARGON BUSTER
Capsaicin - This chemical, found in chillies, binds to a nociceptor that also responds to extreme heat. This is why biting into a chilli can cause pain.
Nociceptors -These are receptors on the pain nerve fibres that act like a lock. Certain keys (irritants, mechanical forces, temperature) open them and set off messages to the brain, signalling pain and tissue damage. Over-the-counter painkillers target nociceptive pain.
Pain nerve fibres - A∂ (A-delta) and C fibres are nerves that carry signals from nociceptors in the skin, muscles and joints to the spinal cord.
Phantom pain -This is the perception of pain in a limb or organ that’s missing. This most often occurs following the amputation of an arm or a leg. It’s devastating for patients, and some theories suggest that it’s a result of altered nerve signals in the brain trying to ‘fill the gap’.
Placebo analgesia -Placebos are substances with no active therapeutic effect. Patients who take them often report improvements in their condition. Placebo analgesia is pain relief from, say, a sugar pill, and neuroimaging has shown that it can work by hijacking an old and inbuilt ‘free pain relief’ system in the brain.
What we still don't know about pain
1
How we detect a pinprick

Using molecular biology and various natural chemicals as ‘probes’, we’ve identified most of the nociceptors in the body that respond to painful events.
However, we’re still missing the nociceptor that detects a painful hammer blow, knife cut or pinprick. Several research groups are on the hunt for this elusive nociceptor.
2
Why some people develop chronic pain

In chronic pain, the A-delta and C fibres often switch on permanently, causing non-stop agony. If we can work out why this happens and manage to prevent it, we’ll have gone a long way to helping millions of sufferers.
Also, we still need to understand why, after the same injury, one person can develop chronic pain, but the other person does not.
3
Where the 'hurt' is in pain

It’s thought that Oscar Wilde once said: “I don’t mind pain, so long as it doesn’t hurt”. Funny, yet spot on.
We know that the perception of hurt emerges from a network of brain regions activating together, but we still don’t know exactly how this activity produces the ‘hurt’ of pain. Brain imaging should tell us more...


