Imagine for a moment that you have a tiny but worrisome lung nodule or, say, a growing bulge in a crucial blood vessel. You have no choice but to continue with normal life: going to work, running errands, paying taxes, negotiating with your kids over screen time. But you’re always living, at least to some degree, under the looming shadow of a medical question mark.
Judy Refuerzo ventured further along that uncertain journey this summer, walking the full length of the Camino de Santiago – some 500 miles and 38 days across the Pyrenees into Spain – to commemorate her 60th birthday. It had been a long-planned trek, one that she tackled with a backpack and a close girlfriend for company. She’s not in denial, she insists, about the malignant cells that doctors found in her breast nearly two years ago.
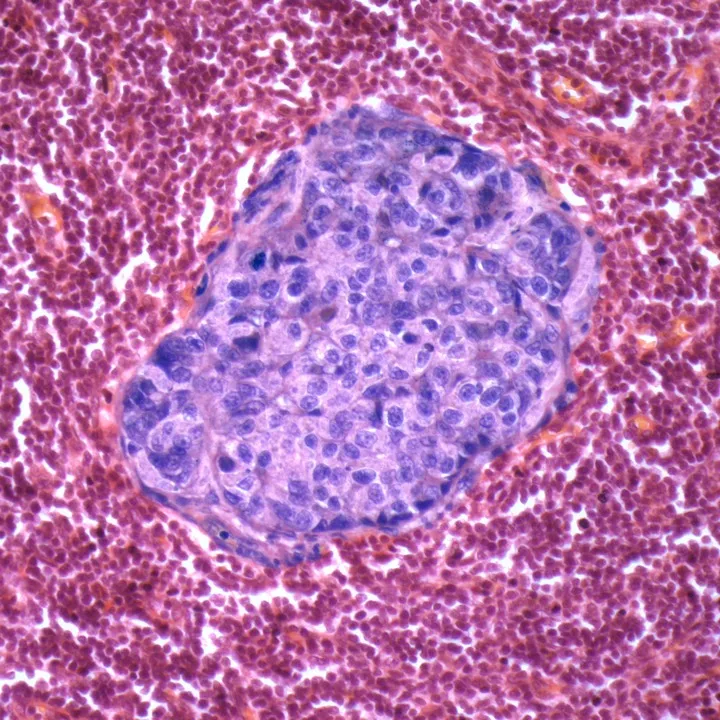
She’s been getting regular imaging tests to make sure that the cells – collectively called ductal carcinoma in situ (DCIS), or sometimes stage 0 breast cancer – have not migrated beyond the milk ducts. But the California yoga teacher has decided against any kind of treatment, including surgery – at least for now. “I just don’t want to be cut open for no reason,” she says.
Through the ages, doctors have sometimes recommended hitting pause on treatment
In the process, Judy has joined a growing group of so-called watchful waiters, snared within a modern-day web of aggressive testing and medical uncertainty.
The concept of watchful waiting (synonymous, for some doctors at least, with ‘active surveillance’) is nothing new. Through the ages, doctors have sometimes recommended hitting pause on treatment. Increasingly, though, more and more people are caught up in a peculiar medical purgatory, particularly in countries like the USA where an emphasis on screening and high-tech imaging to rule out medical problems can cascade into more testing and other uncertainties.
“I think our technologies are moving faster than our ability to know what to do with the conditions we find,” says Shelley Hwang,a breast surgeon at Duke University Medical Center and a prominent DCIS researcher. “And once you know it, you can’t un-know it.”
Sometimes, as in Judy’s situation, people will choose that wait-and-see path. While still quite controversial, some doctors are willing to delay surgery and other treatment for DCIS unless there are signs that the malignant cells are moving into the surrounding breast tissue. In other medical scenarios, patients are told flat out that monitoring is the only immediate option, as it’s too risky to operate until circumstances become more life-threatening.
Medicine has reached a crossroads. Shadows, nodules and other changes can be flagged much earlier, in the maybe-or-maybe-not-worrisome stage. Meanwhile, researchers and clinicians are learning that, for some conditions, less medical care might be better, both in the short term and also possibly over the longer haul. Even some cancer cells, it seems, can flare and fade away.
But that shift in medical thinking raises other big questions: Are some people more psychologically able to cope with medical limbo? Can clinicians identify which patients might better weather uncertainty? And how do doctors counteract that innate human desire to ‘do something’, not only in their patients, but in themselves?
“People don’t like this idea of watching,” says Rita Redberg, a cardiologist at the University of California, San Francisco. “The whole fact that we’ve told you to watch… makes you feel like something bad is going to happen.” Even though, she says, a lot of things that are watched will never progress, there is a drop in a person’s quality of life when they get into a surveillance situation.
If she chose to, Redberg could tout medical credentials that run for pages. She’s a long-standing cardiology researcher, a vocal opponent of inappropriate imaging, and the chief editor of JAMA Internal Medicine.
In the late 1970s, she and her fellow medical students were learning how to perform a physical exam, which meant practising on each other. One student found a lump in Redberg’s neck, which – after more than two decades of monitoring with blood tests – was eventually biopsied in 2000. It was papillary thyroid cancer, the most common form of thyroid cancer. Soon after, she had surgery.
If she had had her biopsy today, Redberg might have had another, albeit controversial, option: to simply monitor her cancer. Surveillance has long been considered an option for low-risk prostate cancer, and now researchers are exploring its use in other cancers, including papillary thyroid, which is, very often, so slow-growing that someone can fare well for years without it spreading.
The whole fact that we’ve told you to watch… makes you feel like something bad is going to happen
Another is DCIS, Judy’s diagnosis. As mammography and other imaging has become more common and more sensitive, diagnoses of DCIS now make up as many as a quarter of breast cancer diagnoses. Previously, it was virtually unheard of.
The question is: how risky is it to leave those cells alone?
Since few women choose surveillance, research answers are limited. But a recent look back at patients treated in Boston proved encouraging. After ten years, over 98 per cent of women hadn’t died from their low-grade DCIS, whether they had had surgery or not.
While the cancer outcomes are crucial, the impact on someone’s quality of life shouldn’t be ignored. Some women who choose surgery, radiation and other measures for DCIS might struggle with related pain and recovery for some time, Hwang says. But without surgery, she counters, “there’s another flavour of misery where you’re just worried every day of your life that you’re going to get cancer”.
Hwang is leading the first large-scale randomised DCIS study in the USA, known as the COMET trial, which will analyse cancer rates as well as the psychological ripple effects. Psychological and quality-of-life aspects also are part of a similarly designed study called LORIS, which was launched in 2014 in the UK.
Prior research shows that women with DCIS harbour similar fears about recurrence and dying as those who have invasive breast cancer, despite DCIS being less serious. “We’ve got a lot of worry going on and we don’t even know if the treatment that they’re receiving actually is of any value to them at all,” says Lesley Fallowfield, the principal investigator on the LORIS study’s quality-of-life assessment.
During discussions after her 2014 diagnosis, Judy’s doctors recommended a myriad of treatment approaches – mastectomy, lumpectomy, radiation and tamoxifen – in various combinations to prevent the malignant cells from spreading. Finally, a surgeon suggested that Judy talk to doctors at the University of California, San Francisco, early proponents of monitoring as an alternative strategy. “He said, ‘They have a different view of DCIS than the rest of the world,’” Judy recalls.
As she mulled over her options, Judy worried about the risk of surgery and radiation, including short-term discomfort and possible longer-term side-effects. Plus, no one could guarantee her that the malignant breast cells would be eradicated for good. Do I want to live my life healthy and feeling good, she asked herself, or miserable and not feeling good, with the same outcome?
Judy, who already avoided meat, has made other changes to her diet since her diagnosis, dropping wheat and dairy. She’s also taking vitamin D to supplement her low natural levels. She believes that many of us periodically harbour malignancies somewhere in our bodies, cells that can be beaten back with exercise, nutrition and other healthy habits. But she also admits to flickers of doubt: “Occasionally I’ll think, ‘Why do I think I’m special?’”
Theresa Monck, a 63-year-old from Brooklyn, New York, is soaking up her first years of retirement, especially the opportunities to travel. But her next lung scan lurks in the back of her mind. The former smoker started getting annual CT scans in 2013 to look for any early signs of lung cancer. Two small nodules were identified. Over the last several years they have not grown, a reassuring sign.
Still, Theresa has pushed for a biopsy. Doctors, she says, have told her that the nodules are too small to risk the procedure, which involves inserting a needle into her lung. “I don’t like having them…” she says. “But what am I going to do?”
Theresa and patients like her are providing some insights into just how much angst men and women living in medical limbo really suffer.
In 2013, the US Preventive Services Task Force recommended CT-scan screening for long-term current and former smokers. (European countries have been slower to conduct such screening outside of research studies, which are ongoing.) The goal is to find cancers at an earlier and likely more treatable stage.
But there’s a significant catch. Anywhere from 20 to 50 per cent of people, depending on the study cited, will have to deal with a false positive, where a nodule is found that, after further testing and scrutiny, doesn’t prove to be cancerous. Sometimes patients won’t know one way or the other for years, but will continue to undergo imaging to see if the nodule is growing.
For some people monitoring can morph into an endless loop, says Renda Soylemez Wiener, a pulmonologist at Boston University School of Medicine. While the typical guidance is to stop after several years if the nodule hasn’t changed, this regular scanning can highlight another nodule, and the clock starts over. “Patients wind up in this prolonged period of uncertainty,” she says.
Do I want to live my life healthy and feeling good, or miserable and not feeling good, with the same outcome?
How much distress those scans generate, though, is still not clear. One study tracked just over 2,800 participants in the US-based National Lung Screening Trial. Researchers found that those who had a suspicious nodule detected (and later ruled out) didn’t suffer any more anxiety than those whose imaging tests didn’t turn up anything.
Joanne Marshall, a former smoker, is among those who might have reason to fuss. Her mother was diagnosed with lung cancer in 2012. Soon after, Joanne got her first scan, which identified three small nodules. But they haven’t grown and neither has her concern. “Some people can be nervous nellies – that’s just not me,” says the 54-year-old, who lives near Los Angeles. “I need to watch it because I would like to have a fighting chance, and I can’t take back the smoking history.”
But Wiener says her research shows that not everyone is similarly sanguine if a nodule is found. Sometimes patients act as though they’ve already been diagnosed with lung cancer, she says. A woman in one of her studies quit her job to find another that would allow more time with her family.
In another study, Wiener assessed the perceptions of 122 veterans whose nodules had been picked up in the course of checking out another potential medical problem. Nearly 40 per cent reported at least mild distress after the nodule was identified; 16 per cent described their distress as moderate to severe.
And even when a doctor says that CT scans are no longer necessary, 29 per cent of patients report being ‘somewhat nervous’ to stop surveillance, and 10 per cent would be ‘extremely nervous’.
Theresa, the Brooklyn retiree, had a similar reaction when she learned that clinicians typically don’t follow nodules that haven’t changed for longer than several years. She’d continue the CT scans, she maintains, even if she had to go to another hospital, and even if her insurance wouldn’t cover them and she had to pay herself. How else would she know if one of those nodules ever began to grow?
Theresa and Joanne both carry several small, relatively low-risk nodules in their lungs. Yet their reactions have been notably different. Fallowfield, the principal investigator on the LORIS study’s quality-of-life assessment, says research indicates that we all have personality filters through which we sift medical information, sometimes in surprising ways.
Years back, Fallowfield was involved with a study which looked at the processing styles of 154 women wrestling with the weighty decision of whether or not to have prophylactic surgery to remove both breasts. Just over half of the women – all of whom faced a high risk of breast cancer based on family history or other risk factors – chose surgery. Most of the rest declined, with a small number delaying their decision for various reasons.
Understandably, both groups reported high anxiety at the start. But among those who chose the double mastectomy, those feelings “by and large” eased over the course of 18 months, Fallowfield says. But they didn’t among those women who opted for surveillance.
How could that be? Researchers found some indications in a ‘ways of coping’ questionnaire that they had asked both groups to fill out in order to gauge how they handled life’s difficulties. The women who chose surgery tended to have a more proactive, problem-solving approach, and likely that helped ease their anxiety moving forward, says Fallowfield.
We all have personality filters through which we sift medical information, sometimes in surprising ways
The women who declined were prone to using “detachment or distraction as a way of coping with life’s traumas,” she says. “These were ostrich-head-in-the-sand-type people.” But that coping mechanism had a crucial flaw. Imaging tests and check-ups kept reminding them of their cancer vulnerability.
Suzanne Miller, a clinical health psychologist who studies medical decision making, believes that the UK women who turned down the operation fall into a subset known as ‘monitors’, one of two coping styles that she first described in the late 1970s. The others – ‘blunters’ – prefer to engage with medical details and discussions on an as-needed basis. “They hear what they’re told,” she says, but are not inclined to dig further.
Monitors are more likely to do research before an appointment and pepper the doctor with questions. They’re also more likely to amplify any medical risks, which can become stressful if they decide on surveillance for a condition such as DCIS, Miller says. They may choose it “on the basis of the rational concrete pros and cons,” she says. “But many of them understand going into it that this is going to have an emotional toll.”
In recent years, Miller has come to believe that monitors can be divided even further by coping style. ‘Non-strategic monitors’ likely haven’t taken steps to mitigate the emotional toll between scans and check-ups. They might continue to fret and stew, which can snowball into regret that they haven’t taken a more ‘active’ step, Miller says. Hence the pervasive anxiety suffered by the women who turned down prophylactic mastectomy in Fallowfield’s study. Another example is men with early-stage prostate cancer who initially commit to surveillance, but eventually go under the knife because they can’t stand the uncertainty.
Judy Refuerzo is what Miller describes as a ‘strategic monitor’, someone who relies on support, self-care and other strategies to dampen their own monitoring tendencies. Along with boosting her nutrition and striving to live life to the max – Judy says she’s probably a bit more spontaneous these days – she tries not to think too much about her cancer risk. Yet she still has scans every six months.
“I’m under surveillance,” Judy says. “I’m not an idiot – I’m proactive.” In February 2016, Judy’s most recent MRI scan showed some DCIS growth, but no signs of invasive cancer.
Miller’s tool, the Monitor–Blunter Style Scale, is one way that clinicians can get a snapshot of a patient’s coping style. It would also be helpful if a doctor could capture a sense of an individual patient’s risk tolerance, says Shelley Hwang, the Duke breast cancer surgeon – something similar, she says, to how financial planners assess whether their client is capable of or interested in taking on additional financial risk.
Patients and doctors caught in this cycle of surveillance are fighting one of the most innate human tendencies: the desire to act, says Paul Han, a physician and researcher who studies medical uncertainty and risk communication. That impulse can infect far more mundane situations than expanding aortic aneurysms or early-stage cancers, Han says, noting that every day doctors must decide whether to prescribe antibiotics to patients with respiratory symptoms.
“Everybody wants something done, when in fact often nothing is really needed except observation and letting things run their course,” he says. “But there is this sort of general impatience in our medical culture, and in our culture at large.”
Han speculates that this discomfort with watchful waiting might figure more prominently in the USA than in countries in Europe and elsewhere where conversations about healthcare costs and trade-offs are more publicly hashed out. Fallowfield agrees, wondering if the US-based DCIS study (COMET) might struggle more than the UK one she works on (LORIS) to recruit patients willing to have their treatment randomly assigned, as Americans tend to be “less risk-tolerant”.
Everybody wants something done, when often nothing is really needed except observation
Fallowfield also echoes other clinicians who worry that misleading medical language can unduly alarm patients, ramping up their perception of their own risk status and thus influencing their treatment choices. When talking to LORIS study participants, clinicians use the term ‘active monitoring’ rather than ‘watchful waiting’. “‘Watchful waiting’ sounds quite passive – you are sitting there waiting for something to happen,” she says.
Using the term ‘ductal carcinoma in situ’ is similarly like waving a red flag in front of patients, Fallowfield says, because it includes the word ‘carcinoma’. If keeping DCIS as an acronym is important, she suggests other terminology, such as ‘ductal changes in situ’ or ‘ductal calcifications in situ’.
In the prostate field, there’s an analogous diagnosis to DCIS, a pre-cancerous condition called high-grade prostatic intraepithelial neoplasia. It’s the word ‘neoplasia’ that “can set off patient alarm bells,” says Ian Thompson, a prostate cancer researcher in San Antonio, Texas.
“Didn’t Ralph Nader call the Corvair unsafe at any speed? The terminology does affect behaviour.” Thompson and other clinicians have proposed a less malignant-sounding, albeit clunky, alternative: IDLE, short for indolent lesions of epithelial origin.
To reduce patient fears, clinicians should do a better job at communicating medical risk, says Renda Soylemez Wiener, the Boston pulmonologist. She points out that just one-quarter of 244 patients diagnosed with lung nodules were able to predict with any degree of accuracy the likelihood that their nodules would prove to be cancerous. Overall they pegged their risk at 20 per cent, but their actual risk based on nodule size was 7 per cent. Nearly three-quarters of them didn’t realise that some lung nodules grow so slowly that they will never prove to be life-threatening.
A surveillance contract could also help avert patient–doctor misunderstandings, says Brendan Stack, Jr,an Arkansas thyroid cancer specialist. A written agreement for patients considering thyroid monitoring could ensure an upfront discussion of the risks involved, he says. It could also lay out the circumstances under which the patient’s decision would be revisited.
Once a patient has ‘self-declared’ that surveillance is the best course, it can be difficult to convince them to deviate, even if the malignancy shows signs of becoming more aggressive, says Thompson. “Changing horses from doing nothing to something is sometimes difficult for people, if you will – to push a reboot to the computer and reassess.”
From Rita Redberg’s perspective, there is one easy way to reduce the expanding pool of watchful waiters: stop searching for medical ills so fiercely in the first place.
She now wishes that she hadn’t dug so far, literally, into her own thyroid.
There’s one easy way to reduce the pool of watchful waiters: stop searching for medical ills so fiercely
After the lump was detected during medical school, a radioactive iodine scan determined that it was a ‘hot’ nodule – one that produces excess thyroid hormone – but likely benign. Redberg did little more to check it out for some two decades, other than periodic blood tests, until her primary care doctor worried that it might be growing. She agreed to a needle biopsy, which she now regrets. Her surgery in 2000 left Redberg with a scar on her neck. Each day, she takes a thyroid replacement pill.
Strangely enough, Brendan Stack has a similar story. He was teaching medical residents about ultrasound technology and they were practising on his neck when they found a thyroid nodule. It was biopsied twice, but cancer still couldn’t be completely ruled out.
Watchful waiting was one possibility. “I couldn’t tolerate that,” Stack recalls. “I said, ‘We’re taking it out.’” In 2006, he had surgery to remove the half of his thyroid where the nodule was located. The pathology showed no signs of cancer. Even so, he has no regrets: “I’d do the same thing today.”
And Redberg? She’s not quite so unequivocal, given how slowly thyroid cancer typically grows. “Probably, on balance,” she says, “I would have been happier not to have known about it.”