Kirk never got over the death of his mother. When she passed away in 2011 after a long illness, the 47-year-old IT specialist kept himself busy by organising her funeral and dealing with the other administrative tasks that come with a death in the family. But while his father and brother managed to pick themselves up and move on, he struggled to come to terms with the loss.
“After the funeral was over there was nothing left to organise or create, and I found myself in a kind of void that just persisted until I was overwhelmed,” he says. “After six months I was still talking about her death, and I wondered whether I should be over it by now. Should I have moved on? Should I be better? But I didn’t really feel that way – I kept feeling worse and worse until I was just chronically sad all the time.”
Eventually, Kirk spiralled into a deep depression that reached into all areas of his life. He signed up for counselling and visited a therapist every week for a year. It didn’t work. His GP prescribed a number of different antidepressants, but they didn’t work either. “The drugs just turned me into a zombie,” he says. “And although I talked through everything else in my life during counselling, I just couldn’t talk about the grief. It was too difficult. When I felt it bubbling up I would just change the subject.”
Every year, thousands of people in the UK are diagnosed with depression and these numbers keep rising. While antidepressants are a common treatment, studies suggest that more than half of all patients don’t respond to the first drug they’re given. A significant proportion of people with depression fail to find something that works for them, ending up cycling through periods of treatment and relapse.
In search of a more effective approach, researchers at Imperial College London have been finding out whether the mind- and mood-altering properties of psychedelic drugs such as psilocybin (the active ingredient in magic mushrooms) could be helpful for treating psychiatric conditions. Led by Dr Robin Carhart-Harris, a team of researchers have been running a clinical trial testing the effects of psilocybin on a small group of people with intractable depression. People just like Kirk.
The psychedelic spa
“We’d been doing brain imaging studies looking at the effects of psilocybin which suggested that it might have antidepressant effects,” explains Carhart-Harris. “We also knew that psychedelic drugs can dissolve the ego [the sense of ‘self’] temporarily. This is accompanied by the possibility of emotional, personal, philosophical and existential insight, so it was a case of joining the dots.”
Spurred on by a previous study showing that people who took psilocybin reported a long-term increase in psychological wellbeing and a trial showing the drug’s benefits for treating anxiety and depression in terminal cancer patients, Carhart-Harris put together a plan to test whether it could relieve treatment-resistant depression.

Despite receiving some funding from the Medical Research Council in 2012,, the proposal was hampered by ethical and regulatory red tape, as well as the challenge ofobtaining clinical-grade psilocybin. But after three frustrating years Carhart-Harris was finally able to start recruiting patients for his unconventional clinical trial, and Kirk was one of them.
“I was open to something potentially a bit more healing than just trying to gloss over the feelings or chemically dull them,” Kirk says. After an initial interview over the phone, he was invited to come to Imperial College’s clinical research facility in London for a longer discussion and a lengthy questionnaire. Next was an orientation session, allowing Kirk to get used to the environment in which the drug would be administered.
He was taught a grounding technique to combat anxiety and stay anchored in reality. Then came a blindfold and headphones playing a specially curated music selection ranging from ambient sounds and tribal rhythms to soaring opera, interspersed with short periods of silence.
“I went into this hospital room and it was done up like a psychedelic spa!” he laughs. “There were throws, imitation candles, aromatherapy machines – it was very relaxing. So, when it came to actually taking the first dose of psilocybin I felt reassured because I’d seen the room and heard the music, I’d been in that space and thought it was a nice environment.”
Tripping on trial
The researchers tested 19 volunteers with two doses of psilocybin – 10mg and 25mg – given a week apart, each with an MRI scan before and afterwards. While the first dose is relatively low so the participants get used to the sensation, the second one packs a bigger psychedelic punch.
“It’s a big trip, and it’s probably more than people would take recreationally,” explains Carhart-Harris. “That’s the kind of dose required to produce ego dissolution,the sense of oneness that has been said to be at the core of what some people describe as a mystical experience on psychedelics. It’s a massive trip, but they’re doing it in a controlled way in a clinical research facility with psychiatrists, beautiful music, low lighting, nice furnishings, and an emergency medical response team on hand in case anything goes wrong.”

For Kirk, this higher dose produced a profound effect. “After taking the higher dose I started seeing this weird Sanskrit writing, then it got a lot busier and more psychedelic,” he says. “The music played a big part of the experience – it’s like a river guiding you through a landscape. I remember an operatic piece that felt like I was being lifted up and it was all washing over me, then it guided me to a sad place where all the grief came up. At one point my eyeshade was so wet I had to wring it out because I’d let go of so much sadness.”
This intense emotional release enabled Kirk to finally address the feelings he had buried since the death of his mother.
“Right afterwards I felt very relaxed and spaced out, and I had a really good sleep that night,” he says. “There was a lot of processing that happened, coming to terms with the grief. There will always be that sense of loss, but I’m not crushed by it like I was before and I’ve become much less withdrawn at work and socially. A week after the treatment I was out shopping with a friend and I just had this sensation of space around me. I realised it was a feeling of optimism that I hadn’t had for so long, and it felt really good.”
Overall, the results of the trial were impressive. Psilocybin caused no significant side effects other than mild nausea and headaches in some people, and didn’t lead to any unpleasant flashbacks. More importantly, it seemed to work. All the participants had a reduction in their depression symptoms, with those who had the most extreme psychedelic experiences having the greatest improvement – an effect that has persisted in the long term. Two years after taking part in the study, Kirk is still feeling well and hasn’t returned to taking antidepressants.
Carhart-Harris also saw a difference in the brain scans of volunteers after they’d undergone the treatment. He noticed that certain networks in the brain seemed to break down under the influence of psilocybin and reformed again afterwards, particularly the default mode network – a system in the brain that is associated with our internal world and sense of self (see box, left). He also saw a boost in responsiveness in a region of the brain called the amygdala, which is associated with emotions – the opposite of the emotional flattening that many people experience when taking conventional antidepressants.
“The default mode network is over-engaged in people with depression and it’s hard to turn it off, so they get stuck in a rut in their own head. When people are in the throes of an intense psychedelic experience the default mode network will be quite markedly disintegrated,” he says, pointing out that the people who showed the most clear reformation of the default mode network after taking the drug were those who improved most after treatment.
“With psilocybin, you take a system that is somehow functioning abnormally and shake it up in a controlled setting – you scramble it up, melt it, shake it up – and then you let it reformat, and maybe it resets in a way that is somehow healthier. There is a loss of sense of self and identity, but what replaces it is a sense of being connected to nature and other people and the Universe,” says Carhart-Harris.
Don’t try this at home
Although the results from the trial are promising, Carhart-Harris cautions against trying psychedelics without medical supervision. For a start, psilocybin and magic mushrooms are Class A drugs in the UK and carry heavy penalties for possession or supply. There are also significant psychological risks.
“Psychedelics induce a state of sensitivity and vulnerability,” he explains. “People are in a state of special psychological plasticity just like children are, and they’re sensitive to context and emotion more than they ordinarily would be. It’s important that they are nurtured and protected – if the conditions aren’t right then the experience can be bad and you can potentially harm people.”
Carhart-Harris is planning a new trial which is due to start recruiting up to 50 patients in early 2018, comparing a single dose of psilocybin with a six-week course of the ‘gold standard’ antidepressant drug escitalopram. He also thinks that psilocybin therapy could be beneficial for many other psychological conditions involving embedded or repetitive thought processes, including anxiety, eating disorders, obsessive compulsive disorder, chronic pain and post-traumatic stress disorder (PTSD). And he’s keen to explore whether it could help prevent people in the early stages of depression from sliding into the kind of deep despair that Kirk experienced.
“Prescriptions of antidepressants are going up year-on-year but a lot of people don’t want to take them – often for valid reasons – so we shouldn’t prevent them from having access to psilocybin treatment,” he says.
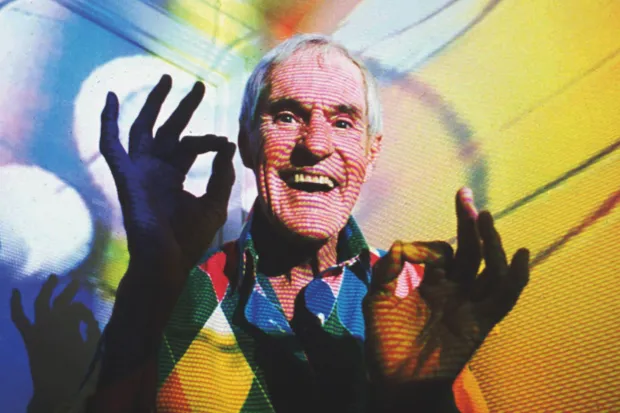
Yet despite the potential of the drug, funders and policymakers remain wary of psilocybin’s reputation, much of which stems from unchecked or unethical research practices dating back decades. For example, the US military is known to have carried out experiments aimed at weaponising hallucinogenic drugs including psilocybin, while Harvard psychologist Timothy Leary gained notoriety for his mind-expanding psychedelic explorations in the 1960s.
Due to the difficulties in gaining funding for his work, Carhart-Harris’s research is currently supported by private donations. A UK-based start-up company, Compass Pathways, is also seeking funding to carry out a larger-scale clinical trial of psilocybin across Europe. But although he’s excited about the potential for psychedelic drugs, Carhart-Harris also knows that the underlying research base needs to be solid, and a lot more work remains to be done.
“I’m not wanting to romanticise these compounds or preach about them – there are risks and things have to be done properly and carefully. This is a real opportunity for a major paradigm shift in psychiatry, but it needs to happen at the right pace. We can’t push it too hard too soon and repeat the mistakes of the past,” he says.
WARNING: Psilocybin and hallucinogenic mushrooms are a Class A drug according to UK law. Anyone caught in possession of such substances will face up to seven years in prison, an unlimited fine, or both. More information and support for those affected by substance abuse problems can be found atbit.ly/drug_support
This is an extract from issue 318 of BBC Focus magazine.
Subscribe and get the full article delivered to your door, or download the BBC Focus app to read it on your smartphone or tablet. Find out more
[This article was first published in February 2018]
Follow Science Focus onTwitter,Facebook, Instagramand Flipboard