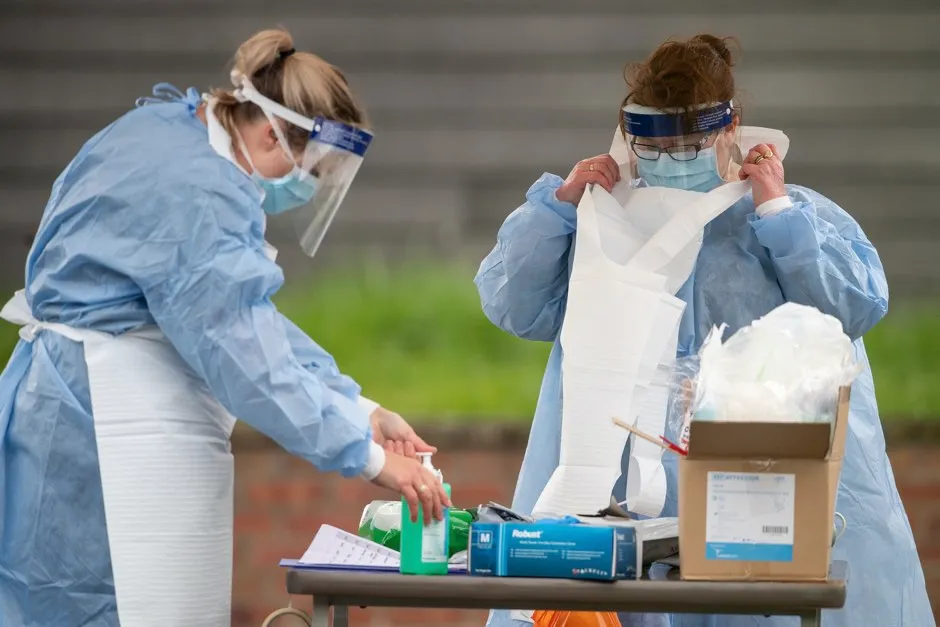
Mass testing is the best approach to tackling coronavirus, according to new research.
Physicists at the University of Aberdeen found severe lockdowns will not create enough “herd immunity” to eradicate COVID-19.
They stressed the importance of “thorough testing combined with contact tracing, isolation of infected individuals and social distancing”.
Lockdowns are probably the most effective way to delay epidemics until faster and more thorough testing or a vaccine is available, they added.
Read more about coronavirus testing:
- Behavioural scientists 'very concerned' about mass coronavirus testing
- Coronavirus antibody tests: How they work and when we'll have them
- COVID-19 antibody test will be ready for distribution in ‘near future’, MPs told
The researchers modelled infections using data from from the early stages of the outbreak in the UK, Italy, Spain, Germany and Hubei province in China.
In the specific outbreaks they modelled, they found that only around eight per cent of the population will have been exposed to the infection, which they said will not lead to the levels of herd immunity required to control and defeat the virus.
The researchers said such a low infection rate could mean that if and when restrictions are lifted, the virus could re-emerge.
The scientists said testing – including people who have not shown any symptoms – is essential to combatting the spread of coronavirus.
Dr Francisco Perez-Reche and Professor Norval Strachan found around 50-80 per cent of the infected population in their models were “silent carriers” who could spread the disease but showed no symptoms.
They predict that in time, a partial relaxation of ongoing lockdowns could keep daily deaths from COVID-19 to fewer than 100 a day.
Dr Perez-Reche said: “Our results demonstrate that the current suppression strategies being employed in Germany, Hubei, Italy, Spain and the UK will not facilitate sufficient levels of herd immunity in the population that would control and eventually eradicate the virus.
“This leaves the risk of re-emergence of the virus once suppression strategies are lifted, similar to second waves of infection observed in 1918 influenza epidemics.
“We predict, however, that partial relaxation of ongoing lockdowns could keep the number of daily deaths to less than 100.”
Read more about the coronavirus lockdown:
- COVID-19: What's the UK's exit strategy out of lockdown?
- Lockdown: why is social isolation so hard?
- Aggressive Wuhan lockdown 'halted coronavirus outbreak' in China
- Which science and tech shows to stream, watch and listen to during lockdown
Prof Strachan said: “Unreported cases act as silent carriers and control strategies would need to account for them or be prone to the risk of re-emergence or ineffective suppression of spread.
“For instance, we predict that isolation of infected individuals can have a limited impact on the suppression of spread unless it includes silent carriers that are currently missed by most countries.”
Dr Perez-Reche added: “In line with previous suggestions, we suggest that thorough testing combined with contact tracing, isolation of infected individuals and social distancing can be more effective to suppress COVID-19 spread than severe lockdowns.
“At present, however, lockdowns are probably the most effective way to delay epidemics until more effective pharmaceutical or non-pharmaceutical interventions – i.e. fast and thorough testing – become feasible.”
Can I get the coronavirus twice?
There have been a few stories in the press of people apparently being re-infected by the coronavirus SARS-CoV-2. These people reportedly became infected and hospitalised, and then were sent home once they’d tested negative for the virus. Then, days or weeks later, they tested positive again.
But this doesn’t necessarily mean that they caught the coronavirus twice.
First, during recovery from infection, a person may have very low amounts of the virus remaining in their body – low enough that our tests can’t accurately detect it. In this case, the person may be sent home on the assumption that they’re virus-free. However, their body may still be fighting the virus, and a resurgence of the virus (and symptoms) can occur, resulting in a positive test. In this case, it would just be one protracted infection, not a re-infection.
Second, we know that in most people, SARS-CoV-2 generates a strong response from the immune system. With the related coronavirus SARS-CoV, this response creates an immune memory of the virus that prevents re-infection for one to two years, and it’s likely that this is also the case for the new virus. SARS-CoV-2 also has a fairly low mutation rate, which means that it (hopefully) won’t change enough that our immune system no longer remembers it (this is what the flu virus does and why we need a new jab every year).
If this all turns out to be true, then it would suggest that re-infections are unlikely and that the cases in the news reflect testing sensitivity. However, SARS-CoV-2 is so new that we won’t know for sure until we’ve found out just how protective our immune response to the virus is, and how long it lasts.
Read more:
