Most of us tend to think that pain is the product of injury or damage to tissue – the knife that slipped, the slipped disc from too much heavy lifting, the baby’s giant head. And there’s a good reason for that: pain, as lived experience has taught us, is an essential warning system, an alarm that sounds whenever we’re experiencing tissue damage or are about to.
But that’s not all that pain is. Sometimes that alarm isn’t giving us accurate or meaningful information; sometimes it’s just a bit behind.
Our experience of pain isn’t nearly as clear cut as, well, a clear cut; instead, our perception of pain is constructed not only from sensory information, but also from context – our circumstances, our needs and motivations, who we’re with, whether we have a sense of agency over what’s happening, and our expectations. And because of this, the thing that we think of as pain is a lot more malleable and perhaps even manageable than we might think.
Pain is not the same as damage
Pain is, for the most part, a great indicator of damage – but not always. For one thing, some things that don’t hurt are damaging; we don’t know we’ve gotten a sunburn until our skin cells begin to die.
Or take an even more dramatic example: after Wilhelm Conrad Röntgen’s discovery that passing electrical current through low pressure gases could give us a glimpse under the skin, doctors, scientists – amateur and professional alike – engineers, and canny entrepreneurs began pointing these new X-rays at anything that would stand still long enough.
Which sometimes turned out to be too long. Early victims of radiation poisoning suffered severe damage to skin and soft tissue and many developed cancers soon after their exposure. But the thing was, radiation exposure didn’t hurt, at least not during the process.
Exposure to radiation doesn’t hurt in the moment because we can only feel what our sensory nervous system is equipped to sense. Science has been able to distinguish between and catalogue a host of different sensory neurons; some are specific to painful mechanical stimuli, for example, crushing pressure, others are sensitive to damaging hot or cold temperatures, and others to specific chemicals, including the chemicals that are released when a cell dies.
Read more about pain:
Activity in the neurons that are sensitive to injury is called nociception, and is part of what allows us to perceive and label different kinds of ‘noxious’ stimuli – to know whether we’ve slammed our hand in the car door or burned it on a hot pan.
As neuroimaging has become more precise – and more affordable – researchers naturally wanted to know what happens in the brain when we’re exposed to noxious stimuli. In 2013, scientists at the University of Colorado made headlines when they published a paper reporting what they described as the ‘neurologic signature of physical pain’, a pattern of neural activation across a network of brain regions that reliably tracked with nociceptive activity.
But here’s where things get really interesting: Neuroscientists can observe this signature in the brain, and patients can report intense pain, without any tissue damage at all.
Consider the story of the builder who stepped on a 15-centimetre long nail. The nail punctured his boot; even the smallest movement was agony. After he was dosed up with some pretty serious narcotics, the team at the hospital was able to extract the nail and lo, “When his boot was removed, a miraculous cure seemed to have taken place,” the British Medical Journal report crowed: the nail had slid between his toes and the foot was entirely uninjured (no word on his pride, however).
Pain doesn’t need tissue damage to be felt – it doesn’t even need tissue. Once considered purely a ‘problem’ of the mind, research confirms phantom limb pain – uncomfortable sensations stemming from amputated limbs – is a form of a neuropathic pain.
This indicates that it is the result of ongoing nociceptive signals from neurons in the spinal cord and brain. In other words, it’s like the phone is ringing, but there’s no one on the other end of the line. Studies show that nearly all patients who undergo amputation report some kind of sensation from the amputated limb, and upwards of about 90 per cent report pain, with 5 to 10 per cent of sufferers rating their pain as severe.
There are several theories as to what causes phantom limb pains; broadly, one pathway could be through increased sensitivity of relevant peripheral or central nerves following the damage to cells that occurs during amputation.
Another pathway, again very broadly, could be an error in cortical reorganisation: when a limb is amputated, the networks in our brain that were responsible for processing sensory and motor signalling in that limb should be taken over and re-tasked by neighbouring networks. The problems arise when they’re not.
We’ve talked a lot about nociception here and that might seem like we’re saying that nociception is pain. It’s not. Though nociception is often part of the experience of pain, it is neither sufficient nor necessary for pain; consider, for example, the pain of depression or grief.
This point was finally explicitly acknowledged by the International Association for the Study of Pain in their definition of pain, updated in September 2020: “Pain and nociception are different phenomena. Pain cannot be inferred solely from activity in sensory neurons.”
Predictive processing
So tissue damage can happen without pain, pain can happen without tissue damage or any tissue at all, and nociception, the thing that seems like it could be pain, isn’t pain. But why? Because our experience of our bodies, our perceptions and the sense we make of sensations, is constructed from much more than what is happening in any one physical part.
Our nervous system is a complex network that is perpetually processing and integrating all the information about our body, doing the business of internal regulation, calibration, and balancing of resources. The goal of this intrinsic – meaning without our conscious awareness – activity is to help us respond and adapt to all that is happening to us or, and this is super important, is expected to happen to us.
Efficient regulation of physiological processes – necessary for our on-going survival – requires learning to not only react to the environment, but to also predict the needs of the body in order to proactively prepare for and meet those needs in the (very) near future.
We do this by constructing and running our own internal model, or simulation, of our lived reality. According to Lisa Feldman Barrett, professor of psychology at Northeastern University, this simulation is essentially neuronal firing based on best guesses of what is about to happen next, kind of like a bridge that forms just as you put your foot down on it.
These simulations are built from all the information gathered and stored from past experiences, along with the present state of the body informed by our representative networks, the mental constructions of our peripheral parts (how you’re able to differentiate between your right hand and your left, for example).
Typically, we’re only aware of this predictive system when our predictions are wrong – when the kerb we step off is much higher than anticipated, for example. A growing number of neuroscientists believe that this predictive processing is how our brain is organised to function – always just milliseconds ahead of our conscious awareness, allowing us to prepare and adapt.

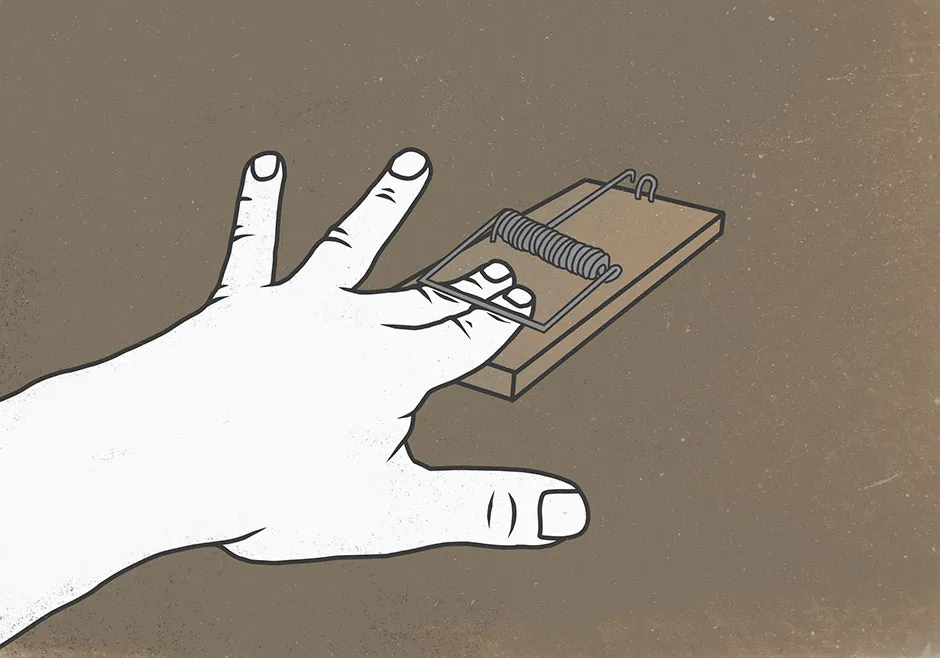
Signals generated from these simulations can be felt just as intensely as the signals we get from the nerve cells that have actually experienced damage. The unfortunate builder who stepped on the nail was really a victim of his own predictive processing and the placebo effect’s evil twin, the nocebo effect.
His foot hurt because all the context clues – specifically, the nail sticking out of the bottom of his boot – pointed towards injury. Instead of waiting for the signals to get passed along up from his foot, his internal simulation of that injury sounded the alarm.
On the face of it, generating the alarm in the absence of injury seems like an inefficient system. But it’s actually pretty useful: A little simulated pain up front can reduce the intensity of the pain that’s predicted to arrive by kickstarting the circulation of our endogenous painkillers, those endorphins and endocannabinoids that are there to keep us moving through injury.
If everything is running as it should, the false alarm is silenced as soon as our systems process that there is no injury after all. But of course, nothing runs as it should all the time and that’s when problems arise.
If we can imagine pain, can we imagine pain relief?
Predictive processing can be responsible for the experience of some pain, but it can also play a big role in relieving it. Perhaps the best evidence for this is in the too-often overlooked therapeutic agent mentioned above, placebo. Placebo – experiencing pain relief or therapeutic benefit based on expectation rather than the ‘real’ treatment intervention – can be powerful.
Studies show, for example, that patients expecting morphine increase circulation of their own endogenous opioids in advance of delivery of the real thing. Increasingly, other kinds of therapies based on ‘gaming’ this predictive processing system are showing promise.
Mirror therapy has been used since the 1990s as a treatment for phantom limb pain, complex regional pain syndrome, and for rehabilitating victims of stroke suffering from paralysis, with some real success.
The treatment can be traced back to the work of neuroscientist VS Ramachandran. Working out of University of California, San Diego in the 1990s, Ramachandran theorised that there could be a way to ‘trick’ the brains of patients suffering from phantom limb pain into believing that their missing limb was restored and able to move, loosening up the discomfort and feeling as though their missing limb was stuck a clenched state. All that was needed to achieve this ‘trick’ was a cardboard box and a mirror.
Read more about the brain:
- This is your brain on love: the beautiful neuroscience behind all romance
- Is it true that we only use 10 per cent of our brain?
Ramachandran took a cardboard box, removed the lid, and slid a mirror vertically down the middle. He cut two holes in the front of the box, one on either side of the mirror. The first subject had lost an arm in an accident years before; he was asked to place both arms – the whole limb and the ‘phantom’ limb – through the holes, and to align his remaining right hand with where he felt the phantom left one was.
Ramachandran then asked him to move both his arms in concert, as if he were conducting a symphony, and watch his reflected ‘left arm’ move. It worked; with his internal model reset, the pain diminished and eventually the impression of the phantom arm disappeared.
With advances in virtual and augmented reality, our ability to manipulate a sense of body ownership is more convincing than ever, offering even more opportunities for pain management. For example, a 2018 study published in Frontiers in Neurology tested VR therapy with two study participants who had previously undergone amputation just below the knee.
In the VR environment, the participants were represented by an avatar controlled by sensors placed on their hips and knee joints; when the user moved so did the avatar. After 20 minutes of playing VR games which required lots of physical movement, and 40 minutes of playing a VR game of their choosing, both participants reported a significant decrease in pain ratings, while their baseline pain ratings also went down over the course of sessions.
Can you reconstruct your own reality?
There are, of course, limits to our ability to construct reality in our favor – a crowning baby is not going to just disappear with a pair of VR goggles or the power of positive thinking.
Pain management cannot be reduced to a chirpy Instagram quote about manifesting your own destiny, and paracetamol does work (although, it should be noted, maybe not as well as two pints of beer for certain kinds of pain, according to a 2017 study) and not only because we expect it to.
Surgical and pharmacological interventions are life-saving and can powerfully reduce suffering, and even then, some pain will still just be the worst no matter what you try.
The most important, not to mention empowering, point is that pain is a complex and multi-layered experience. It’s often driven less by the proximate cause and more by what we think and fear, and both our conscious and non-conscious expectations of it. And that means that in responding to that experience, we have more tools at our disposal – creative, holistic, and not always pharmacological – than we think.
Ouch!:Why Pain Hurts, and Why it Doesn't Have To by Margee Kerr and Linda Rodriguez McRobbie is out now (£18.99, Bloomsbury Sigma).