The realisation that many common diseases are caused by ‘germs’ was probably the most important discovery in the whole history of medicine. It brought about a new technology that was able both to prevent and, eventually, to treat these diseases. It also necessitated new thinking about what disease is.
Germ theory emerged in the 19th Century, but it built on two notions that had earlier incarnations. First, germ theory separated the disease from the person suffering from the disease. Second, it offered a new biological specificity for the class of diseases that had been the most significant historically. These two ideas were fully appreciated only in the second half of the 19th Century.
Doctors traditionally viewed diseases as originating within the human body. The ancient Greek Hippocrates elaborated a theory of four body ‘humours’ that dominated Western medicine for two millennia. These humours (blood, bile, black bile and phlegm) were each produced within the body, and their proper balance constituted health. If there was too much or too little of one or more of them, disease ensued, and the doctor’s task was to restore the balance that was best for the individual patient.
Read more about disease and the human body:
- Sniffing out disease: the power of smell in diagnosing illness
- Vaccines tailored to age group could reduce disease spread 'by almost 50 per cent'
- Five ways deadly diseases carried by mosquitoes have steered the course of human history
This model was challenged by two doctors, Paracelsus (c.1494-1541) and JB van Helmont (1579-1644), who conceived disease as an external ‘thing’ (called an ‘ens’) which could attack any organ of the body. By separating the patient and the disease, they offered a new way of thinking about illness. But although each man had his followers, their ideas did not convince many doctors to abandon Hippocratic humoral principles.
This ‘ens’ remained poorly defined, but it opened the way for the disaggregation of person and disease. The second ultimate insight of germ theory, a new way of classifying disease (disease classification is called nosology), was also elaborated by a doctor with no knowledge of ‘germs’. Thomas Sydenham (1624-89) is sometimes called the ‘English Hippocrates’, because he provided careful descriptions of specific diseases.
In a famous passage, he argued that the symptoms of disease are the same in a Socrates and a simpleton, and that diseases could be classified just like botanists classify plants, which also differ individually. Sydenham didn’t follow up this idea in any detail, but it offered a starting point for later doctors worrying about the names they gave to medical diagnoses. Why do we call this disease measles and that one smallpox?
Miasma and contagion: Two theories to explain disease
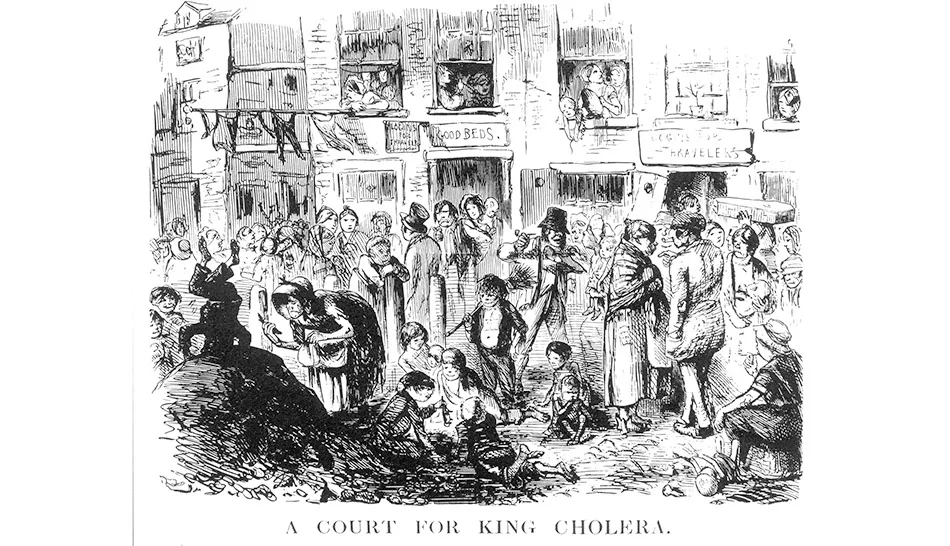
The diseases that the germ theory would eventually help explain and control were those that could often become epidemic, racing through a community or whole country. Plague, smallpox, typhus, scarlet fever and measles were among the scourges that decimated populations. Explaining them was a way to try to prevent their arising and spreading, and two main theories that attempted to do so had been long in contention.
One was miasma, which attributed their prevalence and spread to something in the air: the foul particles of rotting organic matter, such as food, faeces and the other pungent smells that permeated people’s lives in earlier times. This theory accounted for the fact that many people who breathed the same air fell ill at roughly the same time, as an epidemic swept through the community. Removing foul wastes, sweeping streets and cleanliness were all appropriate responses, if this paradigm were the correct one.
Another theory was contagion, which recognised that a lot of diseases like smallpox seemed to be spread person to person, and consequently it was something engendered in the body and passed on to someone in the vicinity. Given this scenario, avoiding the sick and quarantine were in order. The bubonic plague, or Black Death, reminds us that neither theory commanded universal assent.
During the repeated epidemics of plague that swept Europe from the 14th to the 17th centuries, both responses were repeatedly tried. Quarantine and locking up victims and their families in their houses were combined with burning fires in the streets to cleanse the air, and holding nosegays if you were to come in contact with a victim.
Girolamo Fracastoro (c.1476-1553) put the contagionist case in his treatise of 1546, de Contagione. This, combined with his notion of ‘seeds of disease’, has led to some historians seeing him as a father of bacteriology. The reality is much more complex, but Fracastoro’s writings did have influence. Having no microscope, he could not see the ‘seeds’ of which he wrote.
Bacteria were finally visualised by Antoni van Leeuwenhoek (1632-1723), a Dutch draper and lens grinder who produced remarkable magnifications of many objects. As microscopes gradually improved in quality and reliability, many people saw these microscopic creatures and a few tentatively associated them with disease.
Key terms
Nosology
The precise classification of diseases, whereby doctors know exactly the meaning of the diagnoses they give their patients. Germ theory offered a new precision, although many conditions (such as autism) are still difficult to define.
Germ
In medicine, any microorganism causing disease. Before 19th Century research, ‘germs’ were not necessarily living organisms, but could be poisons or bad smells in the atmosphere.
Disease specificity
Historically, diseases were often thought of as highly variable, one disease easily transforming into another – for instance, one kind of fever becoming another during the course of an individual’s illness or as a disease progressed through the community. Germ theory brought a specific cause to these infectious diseases.
Contagia / Miasma
Contagia were the agents by which diseases were thought to spread from person to person, or via soiled clothes or bedding. A few diseases, for instance smallpox and syphilis, were also viewed as contagious. Others were associated with bad smells (‘miasma’ is the Greek word for pollution) that were believed to spread through the atmosphere.
But theirs were always minority opinions, and in the early 19th Century, miasmatic explanations of epidemic diseases still seemed to most doctors to provide the best fit.
The most feared 19th Century epidemic disease, cholera, could be fitted into either the miasma or contagion camp, but John Snow (1813-58), in brilliant investigations of the 1848 and 1854 London cholera epidemics, showed that cholera was spread through contaminated water, not through the air as miasmatists had it.
He did house-to-house surveillance in the neighbourhood of a contaminated public well in Broad (now Broadwick) Street, Soho, and showed that this single well, into which raw sewage seeped, was the source of hundreds of cases.
A wider epidemiological survey looked at the incidence of cholera in the customers of two London water companies. It showed conclusively that the customers of the company selling unfiltered Thames water from downstream, after London’s sewers had drained into it, were about 13 times more likely to come down with cholera than the customers of an upstream company which filtered its water.
In many instances, customers of the two companies lived in the same streets, in identical housing and breathed the same air. Snow analysed the waters chemically and microscopically, and although he found nothing specific to incriminate, he showed that cholera was a disease which was spread by faeces-contaminated water, not foul air.
The emergence of 'germ theory'
‘Germ theory’ was a long time coming, and there were many theories of the role of microorganisms in the causation of disease during the middle decades of the 19th Century. Our germ theory owes most to the work of the French chemist and physicist Louis Pasteur (1822-95).
Pasteur came to microorganisms through his chemical work, and in the late 1850s became convinced that yeast and other living organisms could do things that could not be achieved without life. Crucial in his own journey was his belief that living organisms could not spontaneously generate from non-living matter.

In a series of famous experiments involving swan-necked flasks, which permitted air into his hay infusions but not the dust particles floating in the air, he convinced the scientific community that living organisms had an integrity and continuity that is the special province of biology.
He investigated the role of these tiny organisms in the brewing of beer, the fermentation of wine and the souring of milk.
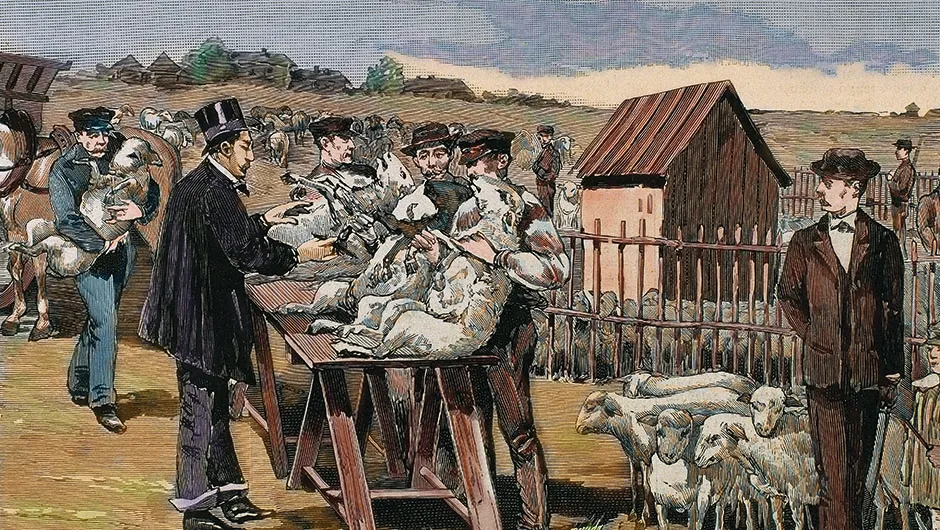
His subsequent work on the diseases of silk worms and farm animals showed the importance of microorganisms in disease processes. This led to his vaccine against anthrax and eventually to his development of a biological treatment for rabies.
Read more about the history of disease:
- Robert Koch: how he identified one of the 19th Century's biggest killers
- 10 key scientists in our understanding of disease
- Epidemiology: A timeline of discoveries
- The experiment that proved bacteria caused disease
Pasteur was the most famous medical scientist of his time, but his methods of growing microorganisms were peculiar to him, and didn’t work very well in the hands of others. His German rival Robert Koch (1843-1910), in contrast, was the quintessential bacteriologist.
He perfected methods for growing pure colonies of bacteria, developed autoclaves for sterilising equipment, introduced photography to demonstrate what he had seen through his microscope, and identified some of the key disease-causing bacteria.
His work on the life cycle of the anthrax bacillus, showing that it had a spore form that could survive in the earth for a long time, put him on the scientific map. In 1882, he announced that he had identified a bacterial cause of tuberculosis, the west’s most lethal disease during the period.
The tubercle bacillus is slow-growing, difficult to culture, and causes a chronic disease (called consumption before Koch’s work) that is totally unlike acute disorders such as typhus, cholera, smallpox and scarlet fever. Koch followed his research on tuberculosis with the identification, in early 1884, of the comma bacillus, which causes cholera.
Neither of Koch’s major discoveries achieved instantaneous assent, but by the 1890s, numerous bacteria had been implicated in disease causation: these organisms satisfied what are still called Koch’s Postulates. The bacteria were in locations in the body that showed they could be part of the disease; they could be isolate d and grown in the laboratory; and they could be injected into experimental animals to produce the disease in question.
Showing that specific bacteria could and did cause specific diseases fulfilled the old dream of Paracelsus and van Helmont, and justified Sydenham’s belief that the course of disease is sufficiently regular that a real classification was possible. It also alerted public health doctors to the fact that individual patterns of spread were the case: cholera through water, typhoid through food, tuberculosis through air-borne droplets and sputum.
Along the way, germ theory also opened up the technology and science to offer prevention through control of water and food supplies, isolation when required, and improvement of people’s working and living conditions. It inspired Joseph Lister’s (1827-1912) ‘antiseptic’ surgery, which developed into ‘aseptic’ surgery, sterilising equipment and trying to keep germs from wounds.

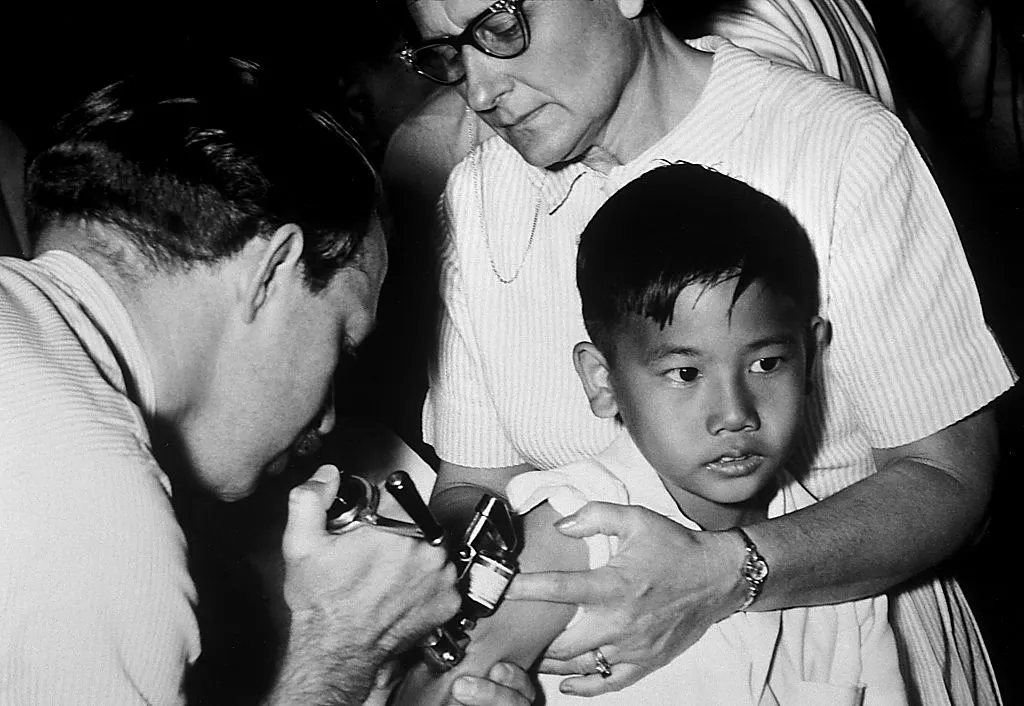
It also provided the hope of vaccines (named by Pasteur in honour of Edward Jenner’s ‘vaccine’ for smallpox, so-called because Jenner used the related cowpox virus – ‘vacca’ is Latin for cow). In addition to anthrax and rabies, vaccines were developed with varying success for cholera, plague and typhoid. New understanding of the body’s response to bacterial invasion led to therapies or immunisations for tetanus, whooping cough and diphtheria.
The battle against disease
The triumph of the science and technology of germ theory by about 1900 turned out to be the beginning, not the end of the battle against diseases caused by living organisms. Rabies is caused by a virus, which is so small that Pasteur’s microscope could not see it.
New techniques and electron microscopes allowed these minute organisms to be identified, grown, studied and, in many cases, prevented by vaccines. Measles, mumps, yellow fever, influenza and German measles have a viral cause and successful vaccines.
But viruses like influenza are also capable of rapid change, making the battle between a vaccine and the new variant a constant one. Bacteria, too, have shown themselves to be wily, as natural selection favours those strains best able to withstand antibiotics and other therapies thrown at them.

Emerging viruses such as the coronavirus, Ebola fever, Lassa fever, West Nile virus and HIV have also reminded us that there are still unpleasant surprises awaiting us out there. Plasmodia (which can cause malaria), rickettsiae (which causes typhus) and other infectious agents also pose threats. Even misshaped proteins called prions, implicated in Mad Cow Disease, pose health threats.
These and a host of other modern health issues mean that many infectious diseases are still to be conquered.