Alcohol is dangerous. Its abuse accounts for around 8,000 deaths in the UK every year, while the societal cost – in terms of the strain on the NHS and the police – is enormous. It costs £3.5bn a year for the NHS to treat alcohol-related illnesses and injuries, while 70 per cent of violent incidents occurring during the evenings, nights and weekends involve alcohol.
Many people are, of course, able to enjoy a drink without coming to any harm, or becoming addicted. But many aren’t: it’s estimated that 9 per cent of men and 3 per cent of women in the UK show signs of alcohol dependence. And if you do get hooked, the prospects aren’t great.
There are many treatment programmes available, but over 80 per cent of people that complete one will be drinking dependently again within four years – and the dropout rate is also high, so the majority of those who seek help won’t even complete a treatment programme in the first place.
But a groundbreaking study currently underway in Bristol may offer new hope. The project is exploring the use of MDMA – 3,4-methylenedioxy-methamphetamine, or ‘ecstasy’ – as an adjunct to psychotherapy, to help addicts come to terms with childhood trauma such as neglect or abuse.
Previous studies in the US have shown that, used in this way, MDMA can be beneficial in treating people living with post-traumatic stress disorder (PTSD). Now the Bristol team, overseen by Prof David Nutt at Imperial College London – the former government drugs advisor who, in 2007, was dismissed from his post on the Advisory Council on the Misuse of Drugs after calling for a more evidence-based approach to drugs policy – wants to see if they can achieve similar results working with alcoholics.
Part of the process
Let’s be clear about one thing: MDMA is not a cure for alcoholism and it’s not simply a case of giving patients a bag of pills and they’ll forswear the booze overnight. Instead, the Bristol study sees psychiatrist Dr Ben Sessa and clinical psychologist Dr Laurie Higbed researching MDMA as part of a programme of intensive psychotherapy, which is only embarked upon after participants have undergone a detox programme to cure their physical dependency. Sessa and Higbed’s programme is aimed at addressing the reasons that drove the patients to alcohol misuse and addiction in the first place.
Drugs for good: LSD
Like MDMA, LSD may have benefits as a tool for therapy. In 2017, a metastudy of LSD research over the past 25 years, published in the journal Neuropsychopharmacology, found that LSD increased feelings of openness, trust and suggestibility, dampened the fear response and enhanced emotional empathy.
It has proved particularly useful in treating anxiety in terminal patients, with as few as two doses causing a reduction in symptoms.
“I did my initial training in child and adolescent psychiatry. I spent 10 years working in an inpatient unit and came across many young people with developing personality disorders. All of them abused, maltreated as children, carrying around a head full of traumatic memories. Many self-harm, some take their own lives before reaching adulthood and many end up dependent on drugs and alcohol,” explains Sessa. “Current treatments for these disorders are very poor. Most psychiatric medications just paper over the cracks. It’s like taking paracetamol if you’ve got a fever – it’ll bring your temperature down, but it’s not going to kill the bug. In psychiatry, the bug is trauma and the only real cure is psychotherapy.”
Many people therefore find themselves turning to drugs and alcohol, which are highly effective at blocking out the pain in the short-term but bring all kinds of new problems with them. But MDMA can help people open up and talk about their most deep-seated problems, so Sessa wants it to be used in conjunction with psychotherapy to provide a better treatment.
Testing environments
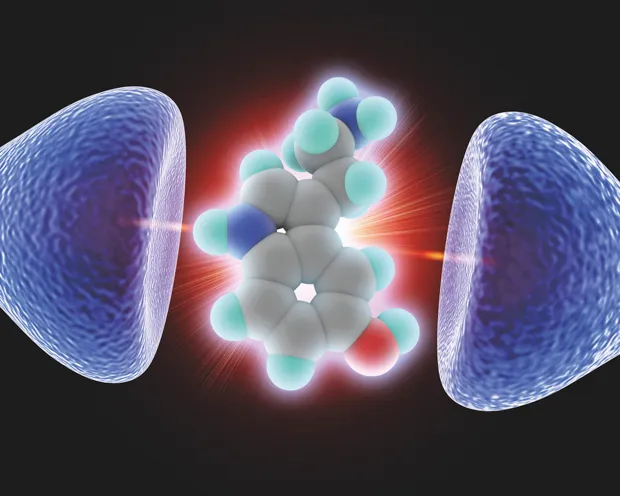
MDMA was first produced and patented in 1912 by German company Merck Pharmaceuticals in an effort to develop an artificial blood-clotting agent. According to records in the Merck archive, the drug was administered to patients in a Berlin hospital but it took until 1927 for someone to notice the similarity between its chemical structure and that of the hormone adrenaline. That’s when the first animal trials were conducted to see if MDMA might mimic the hormone’s effect.
Then in the 1950s, a US chemist called Alexander Shulgin discovered the compound and began to experiment with it as a tool in relationship counselling, which remained its primary use until the early 1980s. But by that point, enough of the substance had leaked out from labs and clinics to be used recreationally that the US government decided to ban MDMA in 1985, putting paid to any genuine research that was being carried out (it had been classified as a class A substance in the UK since 1977).

It’s illegality didn’t prevent the rave explosion of the late 1980s and early 1990s from taking the drug into the mainstream, however, which is something Sessa isn’t entirely happy about. “I see MDMA as a medical tool, and the rave generation as an irritating blip in its history,” he explains. “MDMA is a medical compound.
It started in medicine, it was useful and we were making some great strides. It then stopped for 30 years, but now we’re bringing it back into the clinic, where it belongs. Because from a pharmacological perspective, MDMA is a remarkable compound that works across a number of different receptors.”
MDMA works because it acts upon serotonin receptors in the brain. It increases the levels of serotonin – the ‘happy’ neurotransmitter – to create the drug’s well-known ecstatic or euphoric effects. At the same time, it activates other receptors to provide a mild psychedelic effect – not enough to make the walls seem like they’re melting, in the way that LSD and DMT do, but enough to boost the user’s creative thinking and open their mind to new possibilities.
Paradoxically, MDMA also affects the brain’s noradrenaline and dopamine receptors, which means it has an amphetamine-like stimulant effect while simultaneously inducing feelings of relaxation – this is why ecstasy users often talk about feeling ‘fuzzy’ or ‘fluffy’. It also boosts the brain’s production of oxytocin – the bonding hormone that breastfeeding releases in the brains of new mothers.
A safe space
Essentially, MDMA mutes the fear response while keeping the other cognitive faculties intact. It’s this, says Sessa, that makes the drug such a powerful therapeutic tool. “In some cases, we’re working with people who’ve never experienced a positive mood before,” he explains. “They’ve been living with fear and pain for their entire lives, but now they have this MDMA experience, and they feel good. They feel warm, safe, serene.
“Now a cynic would say, ‘But that’s a drug-induced experience: it’s transient, it’s not real.’ Which is true, but it’s still a valuable experience for someone who’s never had peace in their lives. For six hours, they’ve got peace, and yes it’s a transient, drug-induced peace, but that’s a useful platform because while they’re in that positive mood you can do a lot of good work.”
Drugs for good: Ketamine
Ketamine was developed in the 1960s as an anaesthetic and is still used medically in that context. Recreational use can cause problems with the liver and urinary tract, but the drug can also be beneficial in treating depression, particularly in those who have proved resistant to other treatments.
A 2018 study published in the American Journal Of Psychiatry found that ketamine delivered as a nasal spray could cause an almost immediate reduction in symptoms.
Participants for the Bristol study are recruited from clients of Addaction, a national addiction and recovery service with a base in Weston-super-Mare. They must not be addicted to any other substance (other than caffeine and nicotine) and they must not have taken MDMA in the past six months, or more than 20 times in their lives. There is also a series of tests to weed out anyone who may have other conditions, such as a weak heart or certain psychiatric disorders, that make MDMA use inadvisable.
Once patients have been accepted and have detoxed (either by gradually reducing consumption over several months or after a tapered programme of benzodiazepines over a period of 7-10 days to counter the potentially fatal effects of alcohol withdrawal) they commence their psychotherapy with Sessa and Higbed. The programme involves 10 psychotherapy sessions over eight weeks – only two of which are MDMA-enhanced. There are then follow-up sessions at three, six and nine months.
The MDMA sessions take all day, with patients given a dose of MDMA, followed by a second, smaller dose two hours later. The sessions take place in the Sleep Studies suite at St Michael’s Hospital in Bristol, which is specially re-dressed for the occasion with soft lighting, throws on the bed and rugs on the floor to create a less intimidating environment.
Participants lie on the bed with the two therapists either side of them and don an eyemask and headphones through which a playlist of ambient music specially curated to reflect the peaks and troughs of the MDMA experience is played. And then the talking starts.
“The patients aren’t just lying there in ecstasy, saying ‘I love everything’,” Sessa is keen to point out. “We’re asking them to go to some dark places and to do some very difficult work. But with MDMA, its selective inhibition of the fear response has an extraordinary effect and when we ask about their childhood, they’re amazed at their own ability. They say things like, ‘My God, I can actually tell you all about it’. The MDMA provides a kind of life-jacket that protects you from the fear and allows you to do the psychotherapy. You’ve spent 20, 30, 40 years avoiding these memories, but with MDMA you can go there and talk about it.”
Alternatively, some patients may not talk at all – and that’s okay, says Higbed. “We trust the process and know that they’re having an internal experience. That’s why the patients stay overnight, and why we have another session the next morning before we send them home, where we talk about their experience and help them to integrate it into their lives.”
Risk vs reward
Eyebrows are inevitably raised whenever the use of illegal drugs is discussed. Some question whether MDMA treatment could lead to a new addiction, while others may ask how safe the whole process is.
Sessa is sanguine on both counts. “The risk of addiction is staggeringly low,” he says. Approximately 600,000 people took ecstasy each year between 2000-2015, according to figures from the Crime Survey for England and Wales, “but MDMA dependency is still as rare as hen’s teeth,” says Sessa. “I’ve only heard of one case. Ask any psychiatrist if they have any MDMA addicts on their wards, and they’ll tell you it’s just not on the radar.”
According to Sessa, there have been some 1,600 MDMA sessions given clinically over the past 10 to 15 years and not one single case of dependence has been reported. Mephedrone, meanwhile, appeared as a recreational drug around 2007, and although experts say more evidence is needed to determine if it can cause addiction, a small-scale survey of users in 2011 suggested 30 per cent of them showed signs of dependence.
“As for safety, no medical intervention is ever totally risk-free,” says Sessa. “As doctors we don’t use abstract terms like ‘safe’ or ‘dangerous’. We ask: ‘Is this intervention justified in this particular person at this particular time? Does it come down on the side of benefits and can we keep risk to a minimum?’ That’s the same whether we’re sticking on a plaster or removing your bowel. And when you put MDMA through that analysis – here’s a patient who’s experienced childhood trauma, who has 20 years of alcoholism, who’s had all kinds of medication, who’s been in and out of hospital, been sectioned, attempted suicide… can we justify a controlled dose of MDMA in a clinical situation? It’s an absolute no-brainer. The risk is very, very small compared to the enormous benefits.”
The road ahead
Sessa explains that in rare cases you can get a negative reaction, but they do a lot of physiological screening to avoid that. Plus, all patients have blood tests and an ECG, and are screened for certain mental problems. While the MDMA experience is taking place, the patients are monitored and their blood pressure and temperature is recorded every half hour, to minimise risk.
Still, these are early days and Higbed says that we are still a long way from treatment. The work being carried out in Bristol involves fewer than 20 patients, and is what’s known as an ‘open-label, proof of concept, safety and tolerability study’. This means that everyone knows they’re receiving MDMA, and the real test is to see if this application of the drug has any negative effects. If none are apparent, then Sessa and Higbed hope to get funding for a full-scale, double-blind, placebo-controlled study. And both are hopeful.
Drugs for good: Psilocybin
Magic mushrooms have a similar effect on the brain to LSD, so unsurprisingly psilocybin (the active ingredient) can be similarly useful in treating depression and anxiety.
A 2017 study at Imperial College London showed marked improvement in symptoms and increased brain activity in patients given the drug.
“When I first got involved with this project, I read about the Mithoefer study from 2010, where Michael and Annie Mithoefer in the US used MDMA-assisted psychotherapy to treat Vietnam War veterans with chronic PTSD,” says Higbed. “After 12 weeks they were free of symptoms and they maintained that over three, six and nine months. That’s pretty much unheard of.
“Now in our study, we’ve got two patients coming up to their six-month follow-ups and one coming up to three months, and so far two of them haven’t picked up a drink at all, and one’s only had a single drink on a couple of occasions. That’s already a better success rate than many other programmes.”
Longer term, Sessa imagines a future where MDMA therapy will be available on the NHS. “It’ll never be a take-home drug. But MDMA is on course to be A-approved by the European Medicines Agency in 2021, and after that you should be able to get this treatment legally, on the NHS, delivered through MDMA therapy centres. And the one we’re setting up in Bristol will be the first.”
WARNING: Ecstasy (MDMA) is a class A drug according to UK law. Anyone caught in possession of it will face up to seven years in prison, an unlimited fine, or both.
More information and support for those affected by substance abuse problems can be found at bit.ly/drug_support.
This is an extract from issue 330 of BBC Focus magazine.
Subscribe and get the full article delivered to your door, or download the BBC Focus app to read it on your smartphone or tablet. Find out more
Follow Science Focus onTwitter,Facebook, Instagramand Flipboard