If you’re a fan of apocalyptic disaster movies, you’ll be familiar with all manner of things that might bring about the fall of civilisation: asteroid strikes, deadly viruses, alien invasions, nuclear armageddon. Perhaps even an outbreak of zombies.
Experts now believe that the spread of drug-resistant bacteria is probably the single greatest threat to society – greater even than the dangers posed by global terrorism, climate change and anything you’ll see at the cinema.
There are signs that this ‘antibiotic apocalypse’ is already upon us: in Europe and the US alone, at least 50,000 people die each year from infections that don’t respond to conventional treatment.
What is antibiotic resistance?
Since the discovery of penicillin, bacteria have been able to ‘strategically’ find ways to resist the effects of antibiotics, so that they are not killed, or their growth is not stopped.
These antibiotic-resistant bacteria have been found in every country. If current trends continue, all the world’s antibiotic medicines could effectively be useless in just a few decades.
According to a report by the Review On Antimicrobial Resistance, failure to tackle the problem could cause the world’s population to fall by almost half a billion by 2050 and cost the global economy $100tr.
Read more about antibiotic resistance:
- The nine most dangerous antibiotic-resistant bacteria
- Is antibiotic resistance really as bad as climate change?
Why are antibiotics important?
Antibiotics kill or inhibit the growth of bacteria, helping us to treat both minor and serious bacterial infections.
They are used in all areas of medicine, including the treatment of skin conditions such as acne; more serious infections like food poisoning or pneumonia; and deadly contagious diseases such as tuberculosis and meningitis.
Antibiotics also stop wounds getting infected after an injury or an operation, and help protect people with damaged immune systems, such as patients undergoing cancer treatment or individuals who have recently received an organ transplant.
There are hundreds of different types of antibiotic, from creams to pills to injections, each developed to target different infections caused by different types of bacteria. Since their introduction around 75 years ago, antibiotics have added approximately 20 years to the average life expectancy across the globe.
Life before these wonder drugs was scary – anything that caused an infection could kill you, even a paper cut. In the centuries before modern antibiotics, it’s believed that around 40 per cent of all deaths were caused by untreated infections. And if an infection didn’t kill you, it could leave you scarred or disfigured.
Read more about bacteria:
How do antibiotics work?
Antibiotics are chemicals that disrupt key processes in bacterial cells. To be safely used as a drug, they must specifically affect bacterial cells without damaging human tissue.
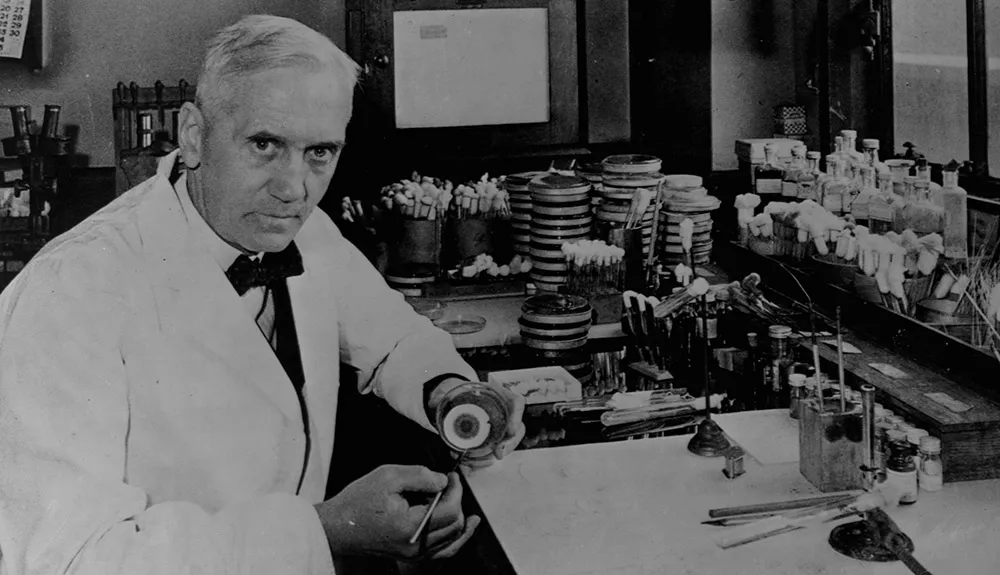
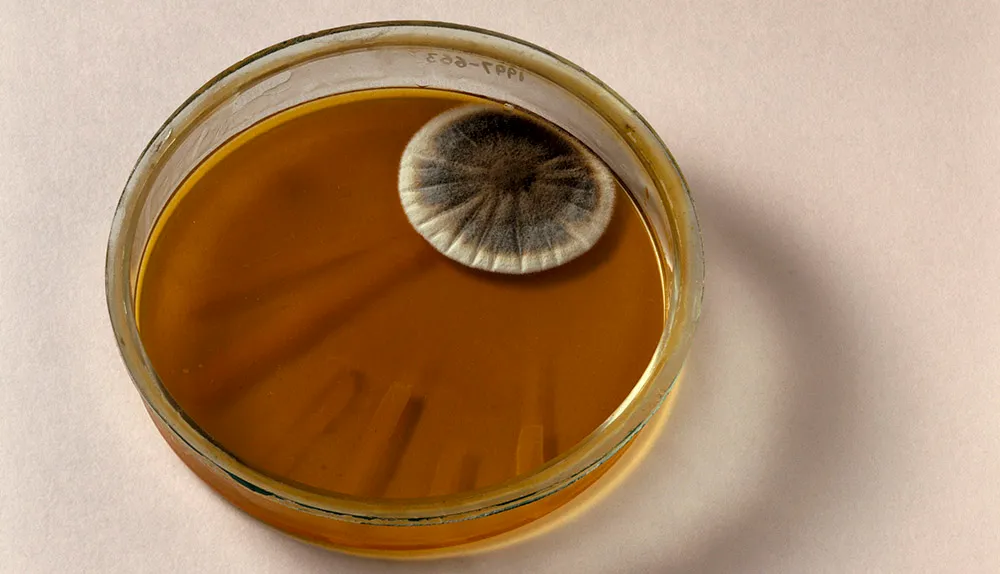
The first modern antibacterial, penicillin, was discovered in 1928 by Alexander Fleming. Produced by a fungus found in mould, penicillin causes the walls of bacterial cells to fail.
Human cells do not have these rigid cell walls, so are unaffected by penicillin, and many similar drugs have been developed over the decades.
Other antibiotics interfere with processes that are essential for bacteria to grow, such as the production of proteins, DNA, or energy.
Scientific terms explained
AMR - AMR, or antimicrobial resistance, is a broad term that includes the emergence of resistance in bacteria, as well as in other microorganisms such as viruses and fungi.
Beta-lactamase -Bacteria that can produce beta-lactamase are a major threat to healthcare systems worldwide. This chemical blocks the action of a key family of antibiotics that act on the bacterial cell wall.
Horizontal Gene Transfer (HGT) -As well as passing on DNA to successive generations, bacteria can also exchange DNA with unrelated microorganisms nearby. This allows them to ‘share’ useful genes, helping resistance spread from one species to another.
MDROs -‘Multi-drug resistant organisms’ are strains of bacteria that are resistant to lots of antibiotics. Some are resistant to ‘last resort’ drugs.
MRSA -Methicillin-resistant Staphylococcus aureus is a common bacterium that has developed resistance to many types of penicillin-style antibiotics. It is one of several strains that have become known as ‘hospital superbugs’.
Mutation - Each time a bacterium divides, its DNA is copied imperfectly and there is a chance it will develop a DNA mutation that is useful – such as resistance to antibiotics.
How do bacteria become resistant?
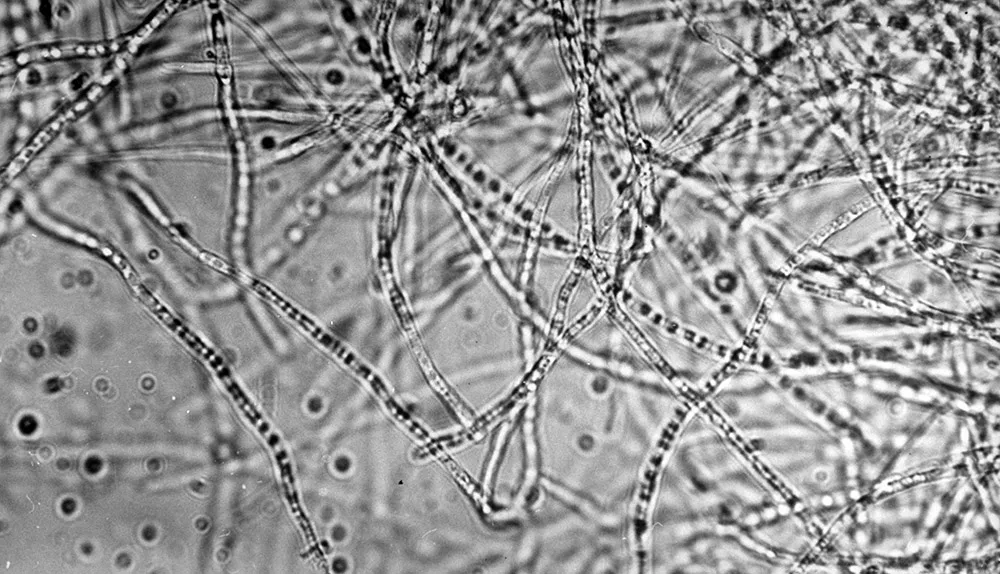
Although it seems like bacteria are in some way ‘learning’ how to fight back against us, the development of antibiotic resistance is an inevitable and natural part of bacterial evolution. Each time a bacterium multiplies, it divides into two and copies its DNA.
Imperfections in this process mean that in a population of millions, billions or even trillions of multiplying bacterial cells, there are lots of ‘mistakes’, know as mutations, in the DNA of each successive generation.
Owing to the sheer number of variants, over time a tiny proportion of individuals will, by chance, develop a quirk that means they are immune to certain antibiotics. A mutation may, for example, subtly change the structure of a key molecule that the antibiotic targets, rendering it ineffective. Or, it may mean the bacteria start producing a chemical that destroys the antibacterial properties of the drug.
In the case of penicillin, many bacteria have evolved to produce chemicals known as beta-lactamase enzymes, which neutralise the drug’s effect.
Once it emerges, antibiotic resistance can jump from one species of bacteria to another. Microorganisms naturally exchange genetic material in a process called horizontal gene transfer – either by close contact or by forming a sort of bridge between each other.
This helps bacteria shuffle their DNA and ‘share’ useful genes, but often causes the genes responsible for antibacterial resistance to jump from harmless bacteria into more deadly types.
As if drug-resistant bacteria weren’t enough of a problem, resistance can also emerge in viruses, fungi and parasites. This is known as antimicrobial resistance, or ‘AMR’. Even insects and weeds are developing resistance to the chemicals we use to destroy pests and keep crops healthy.
How does resistance spread?
Antibiotic resistance becomes a big problem when antibiotics are overused. Using an antibiotic destroys a lot of bacteria in a person’s body – both good and bad strains.
This means bacteria that are resistant to the antibiotic are free to colonise that space and multiply without competition.
This can cause illnesses in the person affected, but also means they will be carrying huge numbers of antibiotic-resistant germs, which are then passed on to other people.
Hospitals act like a sort of transport hub for antibiotic-resistant genes: antibiotics are used heavily, concentrating resistance genes in the ward. These are then passed on to staff, other bacteria and patients.
In a nutshell
Life savers - Antibiotics kill the bacteria that cause infections and diseases. They’re used in billions of operations, and without them, an infection caused by something like a paper cut could prove fatal.
The drugs don't work - As bacteria are constantly multiplying, a small number of cells will emerge now and again with a DNA mutation immunity to an antibiotic. The more drug-resistant bacteria there are, the more dangerous infections become.
The race is on - Scientists are on the lookout for new antibiotics and alternative ways to fight infections. Meanwhile, GPs and patients are being encouraged to curb their use of the drugs. The Longitude Prize is offering £10m for anyone who can develop a cheap, accurate and easy-to-use test for bacterial infections, helping to reduce the number of misdiagnoses and prescriptions.
The more often antibiotics are used, the more likely it is that drug-resistant bacteria will come to dominate in any given location. And it’s not just human medicine that helps spread antibiotic resistance.
In some countries, antibiotics are often routinely administered to livestock to boost growth or to prevent infections spreading throughout herds, which means bugs with genes for resistance are passed back to humans via contaminated meat, animal products, or crops fertilised with manure.
Even in countries with excellent hospital hygiene and strict regulations for preventing the overuse of antibiotics, people and goods from places with poor antibiotic practices are only a short plane flight away.

What if antibiotics stopped working?
First, deaths from bacterial infections like tuberculosis and meningitis would undoubtedly rise. Infections that we don’t currently think of as deadly would also start to cause serious illnesses and deaths.
Even trivial conditions like abscesses or spots would become difficult to treat, meaning that ugly sores and strange skin conditions would become a common sight, like in medieval times.
Read more about the future of bacteria:
But the effect on healthcare would be even more profound.
Each year, billions of operations are carried out around the world, and almost all of them require antibiotics to prevent infections during and after the procedure. One in four births in England is by C-section, where antibiotics protect mum and baby.
Without antibiotics, the risk of dying from an infection after these procedures might mean they simply aren’t worth it. The vast cost of trying to cure difficult-to-treat infections might have crippled many nations’ health services by then anyway. If antibiotics no longer work, we may have to change the way we behave completely.
How worried should we be?
Pretty worried! Many strains of bacteria have acquired resistance to more than one type of antibiotic.
These strains of bacteria, known as multidrug resistant (MDR) organisms or ‘superbugs’, are already putting a strain on the world’s healthcare systems. Prof Dame Sally Davies, former chief medical officer for the UK, said that the golden era of ever-increasing life expectancy may soon give way to an era where mortality rates start to increase.

She told a government inquiry on antibiotic resistance that she was far more worried about “dying in an operating theatre during a routine operation” than climate change.
Hospitals are struggling to rid wards of multi-drug resistant bacteria such as MRSA (methicillin-resistant Staphylococcus aureus), while ‘extensively drug-resistant tuberculosis’ (XDR-TB) has now been identified in 100 countries, causing over 200,000 deaths each year.
In E. coli bacteria, a common cause of food poisoning, resistance to antibiotics is now so widespread that conventional treatment is ineffective in more than half of patients.
And strains of bacteria have been found that are resistant to our ‘last resort’ antibiotics.
Treating patients who have these dangerous bacteria is difficult, hazardous and expensive. Experts have predicted that if trends continue, existing antibiotics could be almost useless in as little as 20 years.

Can’t we just develop new antibiotics?
For decades, resistance was relatively rare and the pharmaceutical industry was constantly making new types of antibiotics.
But by the 1990s, drug companies were starting to run out of new ways to kill bacteria that didn’t involve harming human cells. Many efforts to find new drugs resulted in compounds that were similar to existing antibiotics, and so resistance to these developed quickly, too.
Most of the antibiotics used around the world today are virtually the same as ones developed 30 years ago.

The biggest problem now is money. It can cost anywhere between $500m and $2bn to discover a new drug and bring it to market, yet these new antibiotics will either be saved for use as a last resort or will become useless when resistance to them develops.
This means there is little incentive for pharmaceutical companies to focus their efforts in this area.
However, there is some good news: in 2017 scientists at the Scripps Research Institute in the US announced that they have modified a common antibiotic, vancomycin, so that it now attacks bacteria in three different ways. The researchers say the drug could be used widely without fear of resistance as it’s so unlikely that bacteria ould evade three modes of action at once.
Are there alternatives to antibiotics?
Scientists are starting to combine antibiotics with compounds that disrupt whatever adaptation the resistant bacteria have developed.
For example, if a bacterium has started producing a protein that stops an antibiotic entering its membrane, researchers can develop a ‘decoy’ compound to block that protein. The patient takes a combination of the antibiotic and the decoy, and the antibiotic suddenly works again.
Another alternative to conventional antibiotics is a treatment that has been used in Russia and Eastern Europe since the 1940s but for a long time was not taken seriously in the West.
Known as phage therapy, it uses viruses to hijack bacteria and destroy them from the inside. While it may sound dangerous, the viruses used – known as bacteriophages – naturally attack bacteria and bacteria only.
Other potential avenues for research include drugs that help the immune system to identify and attack bacteria, the use of bioengineered nanoparticles or viruses to bombard bacteria, and the use of probiotic, ‘friendly’ bacteria to outcompete the nasty ones.
The problem with all of these potential solutions? Bacteria could develop resistance to any of these treatments eventually, too.

What else can we do to stop antibiotic resistance?
Due to the ease with which people can travel around the world, containing the spread of antibiotic resistance requires coordinated global action. To preserve the potency of existing antibiotics, their use must be curbed: they must be prescribed only for bacterial infections, and in the proper dose, for the correct amount of time.
Read more about hygiene:
Lots of research is being directed at tests which will allow GPs to quickly diagnose whether an illness requires antibiotics or not, and this should help encourage more targeted use. Other research is looking at ways to interfere with how bacteria swap DNA, to try and eliminate the spread of resistance genes between bacteria.
On an individual level, regular hand-washing and general good hygiene helps reduce the spread of bacteria and therefore the need for antibiotics. People are encouraged not to pressure doctors or pharmacists into giving them antibiotics without knowing for sure what is causing their illness.
In short, the whole of society must start to appreciate these valuable drugs more. The more we use them, the less effective they are.
What we still don't know
How long do we have? - As the development of antibiotic resistance is based on chance mutations and random transfer of genetic material, it’s hard to predict when and where resistance will emerge, and how much time we have left to find solutions.
However, new tools are being deployed to help identify and monitor ‘hotspots’ of resistance around the world.
Can we tackle it globally? - In many ways, our efforts to curb antibiotic resistance have parallels with climate change: the most advanced efforts in one country are worth nothing if other countries continue as they are.
The Western world has made significant progress, but telling developing or poorer nations that they now cannot use antibiotics is not going to be easy.
When will we have new drugs? - It’s unclear how successful research into new antibiotics, and new strategies for extending the life of existing antibiotics, will actually be.
New drugs can take decades to be proven to be safe for widespread use, and cost millions of dollars to develop. After all that research, bacteria may evolve methods to bypass these new systems anyway.