Many of us have heard of the reproduction number, or the R number, of the coronavirus. It tells us, on average, how many people one infected person will pass the disease onto.
The R number changes depending on the circumstances. If people remain socially distant and wash their hands frequently the figure tends to drop, but without these measures it seems the COVID-19 natural R value is three: one person, on average, passes the disease on to three more.
If we can get the R number to below one, the virus will spread to fewer and fewer people and eventually stop transmitting completely.
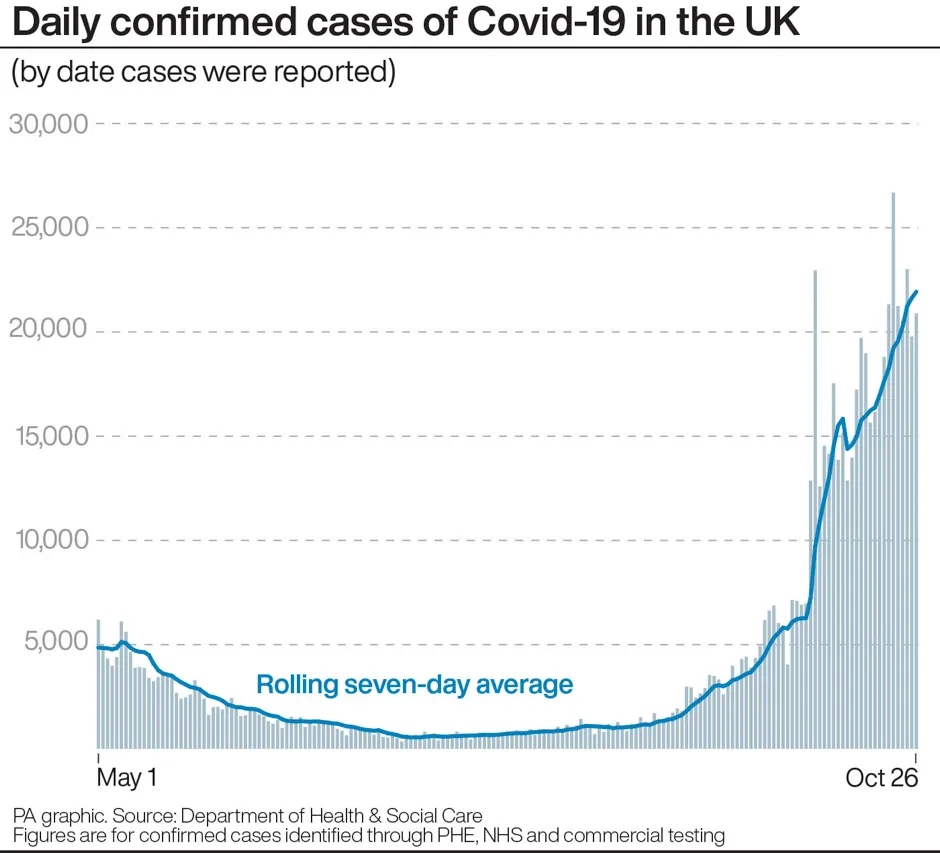
So, why are areas with R numbers close to one still seeing a rise in cases? Over the course of the pandemic, scientists have been gathering data about the coronavirus to inform mathematical models and predict the spread. As we’ve done so, our understanding of how the virus transmits has improved.
Read the latest coronavirus news:
- Public immunity “waning quite rapidly” as fewer than 5 per cent have antibodies
- Coronavirus can survive for 28 days on phone screens and banknotes
- COVID-19 vaccine: Test subjects to be purposefully exposed to virus
“R is a really easy number for people to grasp,” says Benjamin Althouse, a research scientist at the Institute for Disease Modeling. “But it washes over the people who spread a lot, or those who spread very little.”
Research has shown that as much as 80 per cent of transmission events come from just 10 per cent of all infected individuals. This means that most people with COVID-19 don’t seem to pass it on. It was thought to be the same case with previous outbreaks of the SARS and MERS coronaviruses – they are ‘overdispersed’ in the way that they spread, with most cases coming from so-called super spreader events.
Take the example of the so-called Patient 31, in South Korea, an individual who attended several church services before testing positive for COVID-19. These events in February are now thought to have started more than 5,000 cases. More recently in the US, Dr Anthony Fauci called the unveiling of President Donald Trump's nominee to the Supreme Court a super spreader event after 11 people in attendance tested positive.
With information about a virus’s transmission, statisticians are able to calculate a dispersion value: the K number. This can be any number up to infinity. The larger the number, the more consistency there is in the way a disease spreads. The smaller the number, the more it seems that transmission is caused by a few individuals. The K number for SARS-CoV-2 is around 0.1. The SARS 2003 coronavirus has a similar K number of 0.16, while the measles is 0.22. A study in Switzerland looked at seasonal influenza and found a wide range of K values depending on the year, ranging from 2.36 to 53.18.
Althouse explains COVID-19’s dispersion using the analogy of starting a fire. Imagine a pile of logs. Lighting a match and flicking it onto the pile might not set the wood alight. Doing the same with a second match still might not work. But the third match could bring the whole pile to flames. “Now think about dropping someone infected with COVID-19 into a room,” says Althouse.
Identifying the conditions that make the virus overdispersed is key to the fight against COVID-19. To take the above analogy further, understanding that a wet pile of logs will take longer to light, or that a larger match introduces a larger flame, will help inform policies and public messaging to keep transmission down.
Quentin Leclerc, a PhD student at the London School of Hygiene and Tropical Medicine, is one of the authors of a paper outlining the settings thought to foster super spreader events.
“We found that the environments where most of these events happened were indoors, where people were in close proximity to one another, where there was little ventilation, and where people tended to speak loudly,” says Leclerc. But, as Leclerc points out, there is a bias when it comes to identifying where someone might have picked up the virus.
“If you ask someone who's been infected to recall the contacts that they've had, they're more likely to remember when they've been indoors with other people. They're not going to remember that one contact when sitting next to a stranger on a bench in the park.”
Leclerc says that's why it’s not a good idea to try to rank these settings. “There’s no value to saying, ‘oh, going to a food processing plant is more risky than going to a restaurant’. What matters are the characteristics of these settings. Take two restaurants: they're not going to have the same risk because one may have people are seated outside, while the other is intimate and poorly ventilated.”
Understanding this should inform contact tracing efforts, says Leclerc.
Read more from Reality Check:
Currently, if a person tests positive, NHS Test and Trace “helps trace close recent contacts” and “if necessary, notifies them that they must self-isolate at home to help stop the spread of the virus”. This is called forward contact tracing – trying to stop the virus from moving forward and infecting other people.
“Because of the dispersion value, the chances that an individual has infected other people is actually pretty low,” explains Leclerc. “But if you go back one step and try to look at where they were infected, chances are other people were also infected at that setting.”
Another aim of the study was to identify settings which governments or public health institutions should consider keeping closed, or keeping a close eye on, when lifting full lockdown restrictions.
For Althouse and Leclerc, it’s important to say that transmission is mainly caused by super spreader events, not super spreaders. Research has shown that individuals can be infections in the days leading up to their first symptom, which means they could spread the virus without even knowing they’ve got it. “It’s not malicious,” says Althouse. “We all need to be extra careful in our actions.”
Visit the BBC's Reality Check website at bit.ly/reality_check_ or follow them on Twitter@BBCRealityCheck

