From bone marrow transplants, gene therapy and medications inducing a plethora of side effects, current treatment options for those with sickle cell disease, an inherited red blood cell disorder, are few – and often risky.
However, this soon might change. Presenting their findings to the American Chemical Society, researchers are now developing a new drug that could address the root cause of sickle cell disease.
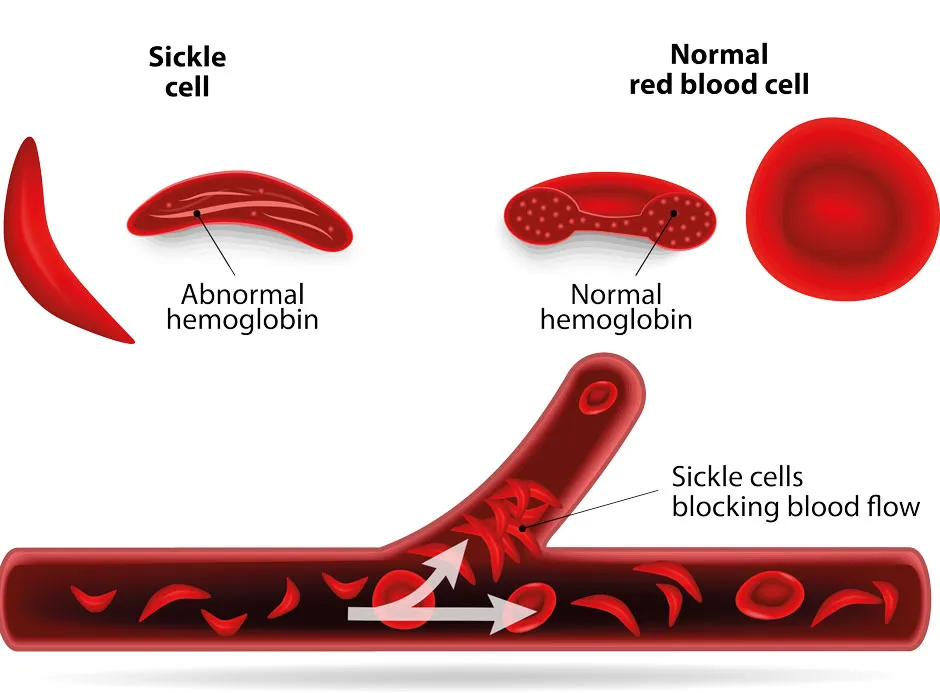
Triggered by a faulty gene, sickle cell disease causes haemoglobin (a protein in red blood cells that carries oxygen) to take on a rigid, sickle-like shape.
As well as meaning less oxygen gets transported around the body, the disease causes red blood cells to die quickly, leading to anaemia.
As these defective sickle cells can get stuck in blood vessels, those with the disease – an estimated 14,000 people in the UK (or 1 in 4,600 people) – are at high risk of stroke, heart disease and kidney failure.
Although the disease is hereditary, sickle cell patients don’t start life with defective haemoglobin. Inside the womb, all humans produce ‘foetal’ haemoglobin that carry oxygen normally. It’s only three months after birth that we start producing ‘adult’ haemoglobin, which are defective in sickle cells patients.
Interestingly, patients still have the potential to produce these healthy foetal haemoglobin cells through bone marrow stem cells.
It’s this last fact scientists used to create their new treatment, which could be formulated into a daily tablet. By attaching itself to a protein inside bone marrow stem cells, the drug can cause the body to produce healthy foetal haemoglobin cells, rather than deficient adult ones.
In an initial trial on healthy adults, the drug was seen to increase foetal haemoglobin levels to around 25-30 per cent of all haemoglobin in the body.
Read more about the science of blood:
- Could I live as a vampire by just drinking blood?
- Is there any part of the body that doesn’t have blood vessels?
"What distinguishes [the new drug] is that we are targeting the root cause of sickle cell disease," says Dr Christopher Moxham, chief scientific officer of Fulcrum Therapeutics, the company behind the treatment.
"Other drugs approved in this space, particularly since 2019, are treating the disease's symptoms, either the anaemia or the vaso-occlusive crises [when sickle cells block circulation]."
The researchers are now preparing phase 2 clinical trials of the drug, which they plan to carry out at the end of 2021. They also hope to use similar medications to treat thalassemia, a blood disorder that reduces haemoglobin production.
Reader Q&A: Can we make artificial blood?
Asked by: Andrew Spero, South Croydon
The idea of having an endless supply of artificial blood to give patients, without worrying about matching blood groups or passing on infection, has fascinated medical researchers for decades. Some substitutes based around haemoglobin (the crucial oxygen-carrying protein in blood) have been developed in the lab. But research published in 2008 revealed that these carried a substantial risk of triggering heart attacks or even death among patients receiving them.
Fortunately, a more promising approach has recently emerged, based on using stem cells to generate real blood to order. Pioneered by researchers in the United States, it has yet to undergo clinical trials, and could yet prove another false dawn. For the time being, the quest to recreate the red stuff coursing through our veins is set to continue.
Read more about the science of blood: