The number of patients reporting symptoms of COVID-19 weeks after becoming ill could be as high as 20 per cent, an immunologist said, as he warned it could place an additional burden on the NHS.
Professor Danny Altmann, from Imperial College London, said a figure of 5 per cent of patients suffering long COVID, reported in October by King’s College London, is lower than what is now being reported.
“Many people would have 10-20 per cent as their range if you look at the papers on how many people are still reporting significant symptoms several months afterwards,” he told Times Radio.
Altmann is calling for long COVID clinics to be opened in the UK, and recently made the case at a World Health Organization meeting for mechanisms to be in place for people to be referred to relevant specialists.
“The point I was trying to make was really a call to arms for some really good solid research and mechanisms here, because there’s no point just having the banner above the clinic if we haven’t got the doctors to sit in them,” he said.
Read more about long COVID:
- Long COVID: Just how common is it?
- Two-thirds have long COVID symptoms 7 weeks after hospital discharge
- 'Persistent' structural changes in lungs could explain long COVID
Symptoms of long COVID include ongoing fatigue, loss of taste or smell, respiratory and cardiovascular problems and mental health issues, which last for at least 12 weeks.
Altmann warned that there is “no absolute correlation” between severe illness and long COVID, adding: “There’s plenty of people out there who barely know they had it and never had a PCR test or antibody test who are suffering massively still from long COVID.
“It really worries me, the kind of burden I’ve been suggesting is equivalent to our NHS burden of arthritis, which is one of the biggest causes on our NHS time and expenditure. It’s a real thing to worry and think about for the future, for patients and healthcare planning.”
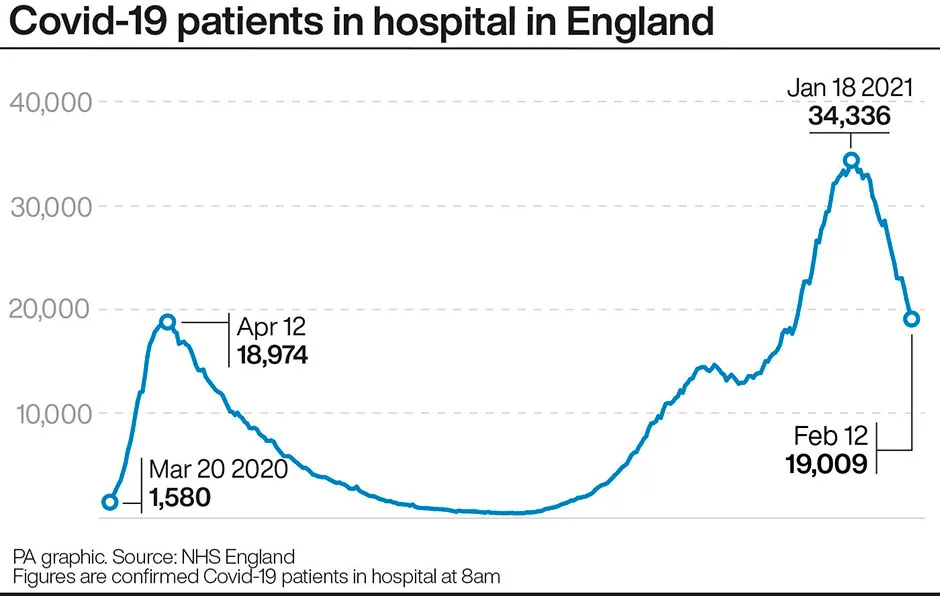
However, he expressed optimism as figures showed there were 25,621 patients in hospital in the UK with COVID-19 as of 9 February, down from a peak of more than 39,000 in mid-January.
Health Secretary Matt Hancock said the UK could live with coronavirus in the future in the same way as flu, and hoped COVID-19 will become a treatable disease by the end of the year.
“I agree with the ‘by the end of the year’ part, I think the jury’s out on what the future will look like,” said Altmann.
On news of the number of coronavirus patients in hospitals going down, he said: “We can’t easily pick apart how much of that is lockdown, how much is vaccination, but it’s certainly both of those things.
“I am cautiously optimistic that we are winning, finally.”
Reader Q&A: Will social distancing measures cause coronavirus to evolve into a more deadly strain?
Asked by: Gary Theobald
Viruses, like COVID-19, evolve rapidly. Each time the virus replicates, mutations can occur in its genome. Most of these mutations have no effect, or are even damaging to the virus. However, occasionally a mutation will arise that is advantageous for the virus. These mutations may allow the virus to grow faster, spread better or evade our immune system. The longer a virus continues to circulate, the greater the chance of these mutations occurring and the virus evolving into a new strain that behaves differently.
However, causing more severe disease isn’t necessarily advantageous to the virus. One of the reasons the COVID-19 virus is so difficult to contain is that it spreads very well before people become sick. If the virus spreadswhile causing more severesymptoms, people with COVID-19 would likely stay home instead of going out (reducing transmission) and would seek medical attention (enabling more effective testing and contact tracing). Sometimes mild viruses are the most difficult to eliminate.
Because the COVID-19 pandemic has been so difficult to contain, we have all had to take precautions, such as social distancing, washing hands and wearing masks. Each of these individual precautions limits the amount of virus that can spread from one person to another. These actions could put pressure on the virus to evolve, possibly resulting in mutated strains that are more transmissible and more difficult to control (though not necessarily deadlier). However, by combining all of these precautions, together with strong public health infrastructure (such as test and trace), we can still effectively stop the transmission of COVID-19, even if it evolves into a morevirulentstrain.
Read more:
