Scientists from Harvard University and MIT have developed a new test that can determine which COVID-19 variant you have, using 3D-printed components and costing as little as $2 (approx £1.44) per device.
Details of the diagnostic device, along with templates for 3D-printing, have been published online. The team behind the test say they wanted to create something simple, that could, for example, "be built by a doctor in Zimbabwe and 3D printed within their facilities". It runs on batteries and gives results in one hour.
The test can successfully identify the Alpha, Beta and Gamma variants in the spit of a patient, and the researchers say they are developing the device to detect the Delta variant.
Should any new variants emerge, the team could turn around a specific test for the strain in just two weeks. The likelihood of this happening, experts have previously said, depends on the number of people getting infected. As more countries ease restrictions, it is likely that more people will get infected. This means there will be more chances there are that the virus will change in a way that does affect the COVID-19 disease, creating a new variant of concern.
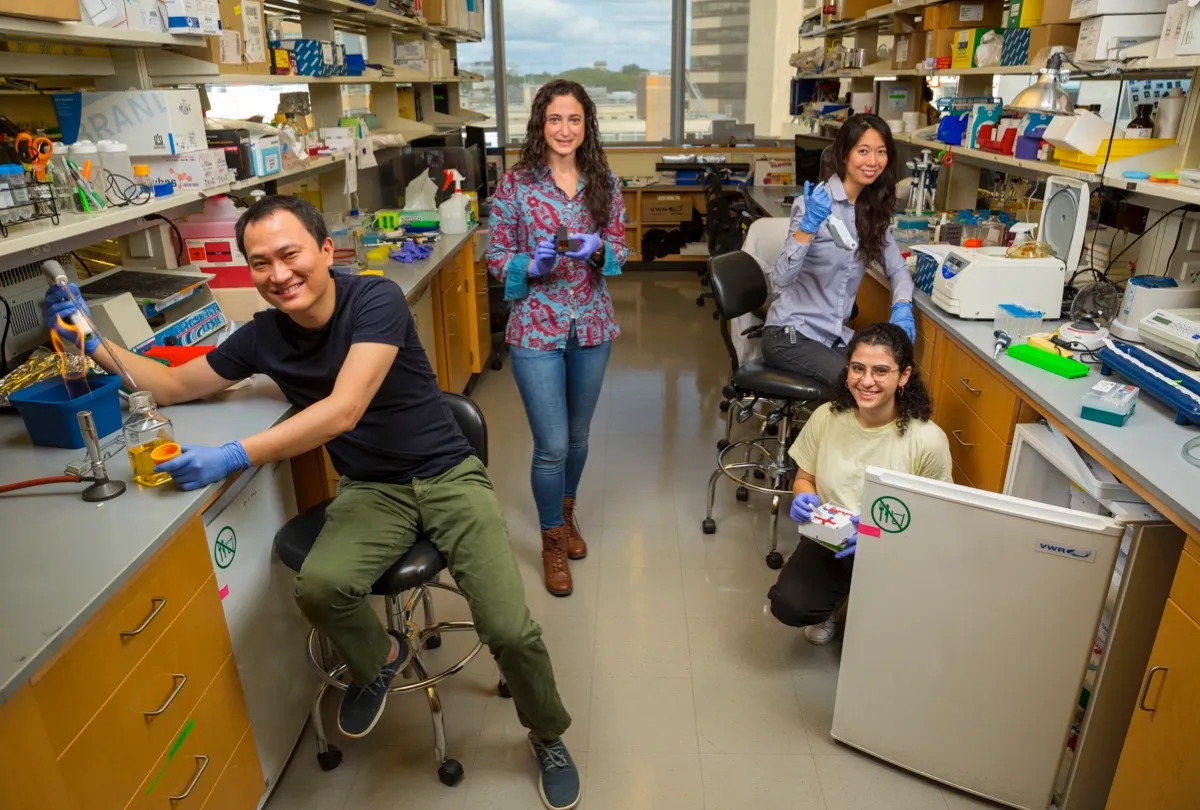
All four co-authors of the research spoke to BBC Science Focus to explain everything you need to know about the new COVID-19 variant test.
How does the COVID-19 variant spit test work?
The test uses the scissors from scientists' molecular toolbox: CRISPR technology.
"CRISPR is a part of the bacterial immune system that has evolved to detect and cut DNA," explained Dr Xiao Tan, one of the four first authors of the research. "For the bacteria, it's a way for it to defend itself. What we've done is co-opt that to detect things that we're interested in."
Unlike some CRISPR technology, the scissors used in the spit test aren’t just one-cut-wonders. Called SHERLOCK – which stands for ‘specific high sensitivity enzymatic reporter unlocking’ – it can actually detect the presence of COVID-19.
The researchers worked with Dr Jim Collins, one of the co-founders of the SHERLOCK technology, to design their device. When SHERLOCK finds a particular spike protein specific to the variant in question, it activates an enzyme, which goes on to creates the fluorescent light that indicates the test is positive, said Devora Najjar, co-first author. “So it’s only if the CRISPR finds the [COVID-19 virus] will it start releasing the fluorescence. If not, you won’t get any fluorescence.”
More coronavirus news:
- COVID-19: Childhood short-sightedness rise linked to lockdowns
- Bizarre ‘alien simulation’ behavioural study shows how COVID-19 panic buying was natural human response
Taking the test is simple and there's no training required, said researchers. First, spit into the sample prep chamber. Turn on the heat and wait for around three to six minutes for the saliva to spread across the filter.
Then, pick up the filter and move it into the reaction chamber column. Push down to add the spit to three small pipettes, which each contain SHERLOCK technology specific to different variants.
An hour later, you'll either see a fluorescent light – bad news – or no light at all. An accompanying smartphone app can also read the result.

The spit test uses minimal instruments, which is why the researchers have named it miSHERLOCK. Compared to at-home PCR tests, the miSHERLOCK device is simpler and cheaper, say the researchers.
"I'm not sure how that works in the UK, but in the United States, just mailing samples like the ones that have been approved by the FDA, costs $120," said Tan.
For the miSHERLOCK test, one device costs around $15. "But if you reuse some of the components, you can actually get that down to maybe $6," explained Tan. "Then we calculated what it would cost a commercial supplier, and you could probably get this thing down to $2-3 per test.
"That's for all the components that you need to give you an answer right then and there, without having to wait 72 hours turnaround for the mailing process."
Can the spit test detect the Delta variant?
In the research, published in Science Advances,the team tested the device against the Alpha, Beta and Gamma variants. They say they are working now to target the Delta variant.
"When we started this project a few months ago, we were looking for the strains that are no longer the top variants of interest," said Najjar. "It speaks to the rapidly changing nature of the pandemic, and how we have to be creating systems that are just as agile as the virus."
Read more about COVID-19 variants:
- Lambda COVID variant: All you need to know about the new UK coronavirus strain
- Everything you need to know about B.1.617.2, the Delta variant of coronavirus
The tubes within the reaction chamber are called assays, and they can be individually designed to target a very small, specific part of a genetic code.
“You can think of the device almost like a miniature coffee machine with different coffee pods. Except we’ve designed each pod, each assay, so they contain these CRISPR enzymes, each one specific for the gene that we're looking for,” explained Dr Rose Lee, another of the study's first authors and an infectious disease specialist at Boston Children's Hospital.
The team currently have developed one 'pod' that can generally detect the COVID gene, and others that detect specific genes for the spike proteins on COVID variants.
Each assay takes roughly two weeks to create – so every time the DNA of a new variant is identified, the team could turn out a new 'pod' 14 days later.
Why do we need to know which variant a person has?
As the virus has mutated it has become more infectious, and further variants could prove to be more deadly.
"Knowing what variant you have could be significantly relevant, because it changes how we think about therapies that we might use for the patient, such as treatment using antibodies," said Lee.
In the case of Delta, one study recently published has suggested that the strain was resistant to neutralisation by several types of antibodies, and that one single dose of the Pfizer or the AstraZeneca coronavirus vaccine had "a barely discernible inhibitory effect on the Delta variant", though two doses did neutralise the virus.
It also helps countries keep track of the variants currently of concern in a population.
"Variant tracking is usually done by sequencing very few samples and then extrapolating from there to get an idea of the whole population," explained Dr Helena de Puig, co-first author.
While the miSHERLOCK device doesn't do sequencing, meaning it cannot pick out a previously unknown strain, it provides data that can be used to track the spread of known variants.
When will people in the UK be able to buy the spit test?
This research now needs manufacturing on a large scale, and approval from bodies like the FDA, before it can be mass-marketed. The team have stressed that their lab does not have the capability to sell the devices and get the FDA approval.
"To commercialise an assay usually you need the manufacturing capability as well as the approval from the FDA," said de Puig. "We would love to see this academic work used in the clinics, and if there are manufacturing facilities that would like to develop it, we would be very, very happy to help them."
The team do hope that this can be used around the world to help populations manage the spread of COVID-19.
"It is very easy for us to make the components, the only thing that needs to change the small part that targets a particular spike on the variant," said Tan.
"In fact, [the device] doesn't even need to be limited to COVID. There are many other infectious diseases where there's viral particles in the saliva that this could be used for as well. We haven't necessarily tested those, but there's no reason why it wouldn't work."
About our experts
Dr Helena de Puigis a postdoctoral researcher who looks at building molecular diagnostic devices at the Wyss Institute for Biologically Inspired Engineering in Harvard University.
Dr Rose A Lee is based at Boston Children's Hospital, where she works as an assistant in paediatrics within the division of infectious diseases.
Devora Najjar is a research assistant at the Massachusetts Institute of Technology (MIT), primarily focusing on bioengineering, participatory environmental monitoring, and education.
Dr Xiao Tanis a clinical fellow at the Wyss Institute and an instructor of medicine in gastroenterology at Massachusetts General Hospital.
