The COVID-19 pandemic has had a global impact, but its effects have hit some groups harder than others.
In the United Kingdom, more than 40,000 people have so far died from COVID-19, with people from black, Asian and minority ethnic (BAME) communities disproportionately affected.
A 19 June report from the Office for National Statistics (ONS) found that black men are more than three times as likely to die from COVID-19 as white men, while black women are almost 2.5 times as likely to die as white women. People of Bangladeshi, Pakistani and Indian ethnicity are also significantly more likely to die from COVID-19 than white people.
A Public Health England report published on 2 June found that people from BAME backgrounds are also more likely to become infected with the coronavirus in the first place. For example, black ethnic groups are around two to three times more likely to be diagnosed with COVID-19 than white groups.
Read more about COVID-19:
Similar patterns have been seen within BAME communities in the US, particularly among African Americans.
“The pandemic has really exposed the vulnerability of certain communities because of the way in which people live, and the way in which societies engage,” says Dr Clyde Yancy, Professor of Cardiology and Medical Social Sciences at Northwestern University, US.
There’s likely to be a complex web of factors at play.
One important statistic is that BAME groups are more likely to live in urban and deprived areas. The effects of COVID-19 are more pronounced in these areas, possibly because people are living in closer proximity and/or have reduced access to healthcare.
BAME groups are also more likely to live in multi-generational and multi-family households, which also favour the virus’s spread.
But even after adjusting for geographical region, population density, and socio-demographic and household factors, the ONS report still found that black men are twice as likely to die from COVID-19 as white men. And the raised risk for black women, and Bangladeshi, Pakistani and Indian men, also remains.
Underlying health issues could be another factor. COVID-19 is deadlier for those with existing medical conditions such as diabetes, obesity or cardiovascular disease.
These conditions are more prevalent in certain ethnic groups: black and south Asian people, for example, have higher rates of diabetes than the general population, while older Pakistani men have especially high rates of cardiovascular disease.
Read more coronavirus news:
- New saliva test for COVID-19 to be trialled in Southampton
- Vaccine researchers looking for trial volunteers
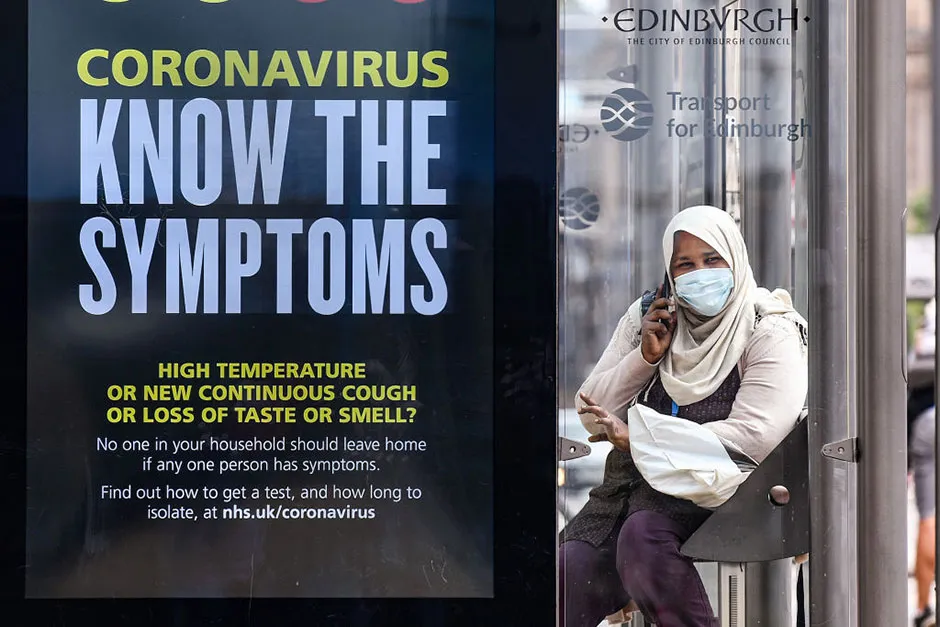
Another key variable is occupation. Key workers – carers, nurses, doctors, security guards, bus drivers – face some of the highest levels of exposure to the disease, which puts individuals and their households at risk, and certain BAME groups are more likely to work in these roles.
An Institute for Fiscal Studies report led by Lucinda Platt, Professor of Social Policy and Sociology at the London School of Economics, looked into this in more depth. She and her co-author Ross Warwick found that working-age black Africans are 50 per cent more likely to be key workers than working-age white British people.
Black African men are also 310 per cent more likely than white men to work in health or social care. And the Indian community make up three per cent of working adults, but around 15 per cent of doctors.
Platt and Warwick say that this “clustering of some minority groups in key worker occupations” is likely to be one of the contributing factors to the disproportionate BAME deaths.

Another open question is whether certain BAME groups could have a genetic susceptibility to COVID-19. However, Yancy cautions against looking for a biological explanation – he believes that the differences in death rates are “less a function of biology and more a function of sociology.”
He notes that there are few health conditions with a strong biological connection to ethnicity. Usually, he says, there are underlying economic or social issues that can explain any differences in disease prevalence or death rates.
When the first Public Health England report was released, it was criticised for not providing any recommendations to protect ethnic communities. But a follow-up report released two weeks later shared seven recommendations, including improving data collection on patients’ ethnicity, carrying out risk assessments for BAME key workers, and developing culturally sensitive health messaging.
Read more fromReality Check:
- Faster-than-light travel: Is warp drive really possible?
- Peaceful protests: Are non-violent demonstrations an effective way to achieve change?
The report said that “historic racism and poorer experiences of healthcare or at work may mean that BAME individuals are less likely to seek care when needed”. It also flagged up lack of trust as an issue, with some BAME individuals worried about being deported if they went to hospital for treatment.
Platt, Yancy and other researchers are keen to see policies which address these issues. More collaboration with BAME communities, for example, could help to develop clearer messaging around COVID-19, and healthcare in general, which would be one way to build up trust and reach those for whom English may not be a first language.
And improved data collection, including the introduction of ethnicity on death certificates, would help to monitor BAME health over time, and make it easier to spot any patterns that need looking into.
“It’s not one big fix,” says Platt. “It’s looking at all the different elements of the system.”
Visit the BBC's Reality Check website at bit.ly/reality_check_ or follow them on Twitter@BBCRealityCheck
