The genomes of thousands of patients with coronavirus will be sequenced to understand how a person’s genetic make-up could influence susceptibility to the virus.
The study will sequence the whole genomes – the genetic code – of up to 20,000 people who were previously in intensive care or who are currently in intensive care at 170 NHS units across the UK.
Patients will have their results compared with 15,000 people who have suffered only mild or moderate symptoms.
Experts hope to explain why some patients with COVID-19 experience mild infection, but others require intensive care or go on to die.
The team also hopes the knowledge gained will help the development of treatments to fight COVID-19 and inform future clinical trials.
Part of the study will also focus on children and young adults severely affected by COVID-19.
It is hoped all patients going into intensive care – with their consent or the consent of their next of kin – can be studied.
Read the latest coronavirus news:
- Pregnant women 'not at a higher risk' of severe coronavirus
- New coronavirus knowledgebase uses AI to accelerate COVID-19 research
- Coronavirus 'targets proteins' found at higher levels in men with heart failure
For the research, Genomics England has partnered with the GenOMICC consortium, which includes NHS organisations and academic institutions, genetic analysis firm Illumina, the NHS and the University of Edinburgh.
Health and Social Care Secretary Matt Hancock said: “As each day passes, we are learning more about this virus, and understanding how genetic make-up may influence how people react to it is a critical piece of the jigsaw.
“This is a groundbreaking and far-reaching study which will harness the UK’s world-leading genomics science to improve treatments and ultimately save lives across the world.”
Some £28 million has been pledged for the project by Genomics England, UK Research and Innovation, the Department of Health and Social Care and the National Institute for Health Research.
Illumina will sequence all 35,000 genomes and share some of the cost.
So far, DNA samples have been collected from almost 2,000 patients.
How to stay safe during the coronavirus pandemic:
- Coronavirus: Should we all wear face masks?
- Is hand-washing really the best thing we can do to stop the spread of COVID-19?
- 5 mental health apps to help you through the coronavirus crisis
Professor Sir Mark Caulfield, chief scientist at Genomics England, said: “For the first time in a generation, we face a global viral pandemic that is life-threatening for some people, yet others have a mild infection.
“By reading the whole genome, we may be able to identify variation that affects response to COVID-19 and discover new therapies that could reduce harm, save lives and even prevent future outbreaks.”
Dr Kenneth Baillie, chief investigator at the University of Edinburgh, who is leading the study, said: “Our genes play a role in determining who becomes desperately sick with infections like COVID-19.
“Understanding these genes will help us to choose treatments for clinical trials.”

Public Health England and the Sanger Institute are already sequencing the genome of the virus itself and it is hoped information from the two studies can be linked up.
This may give insights into how patient and virus genomes act together to influence how the patient responds to the virus.
Illumina has laboratories in Cambridge. Previous work has included the 100,000 Genomes Project together with Genomics England and the NHS.
The data will also be used to inform the global planning for possible future waves of the pandemic, and for new pandemics in the future.
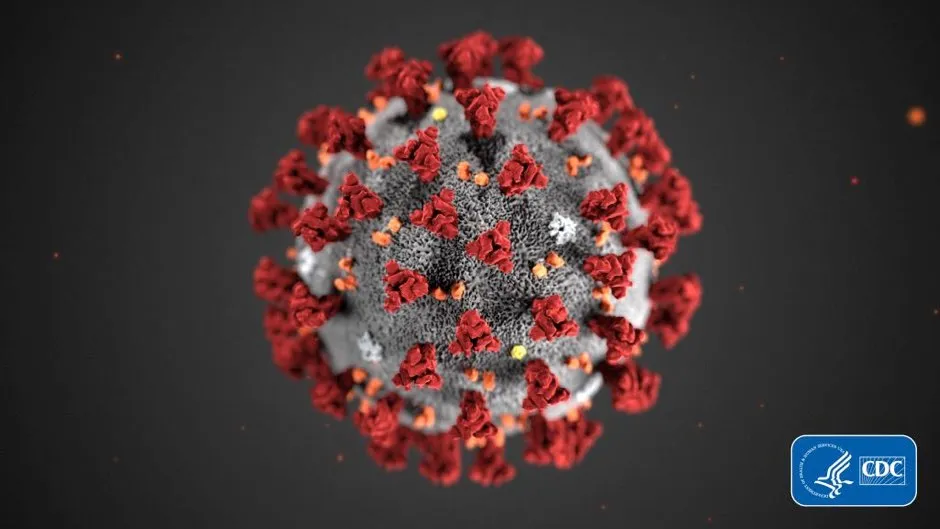
What does the novel coronavirus look like?
Coronavirus is an ‘enveloped virus’. This means it has a protective outer layer known as a ‘lipid bilayer’. The molecules making up this layer are shaped like a tadpole, with a water-loving (hydrophilic) round head and a water-hating (hydrophobic) tail.
These molecules arrange themselves into a ‘bilayer’: two layers piled on top of each other into a sheet, with tails pointing inwards and heads pointing outwards.
The molecules are pulled closely into each other to protect the hydrophobic tails from the water in your respiratory droplets when you cough or sneeze.
The hydrophilic heads are very ‘sticky’, meaning the virus is very effective at sticking to your hands – perfect for a microbe that’s trying very hard to infect you.
Soap molecules also have this tadpole structure, which is what makes it so useful.
Read more:
