A contact tracing app could help stop the spread of coronavirus but 80 per cent of smartphone owners would need to use it, new research suggests.
A study by Oxford University’s Nuffield Department of Medicine found wide adoption of the app and speed of use are crucial factors in stopping the spread of the virus.
The experts, who are advising the Government and the NHS on the development of a UK contact tracing app, said basing an app around symptoms rather than waiting for test results could make a crucial difference to stopping the spread of COVID-19.
Read more about the spread of COVID-19:
- Coronavirus transmitted two to three days before symptoms show
- Coronavirus: Will COVID-19 become a seasonal virus?
The app would alert users if someone they had come into contact with had tested positive for the disease, and encourage them to take precautionary action.
Dr David Bonsall, co-lead on the research and a clinician at the John Radcliffe Hospital, said: “Initiating contact tracing based on symptoms makes sense epidemiologically because it’s fast enough to reach people before they transmit.
“Our simulations predict loss of epidemic control when tracing is delayed to wait for test results, and overall results in more deaths, and more people in quarantine.
“You achieve the best of both worlds when virological tests are used to follow-up and promptly release people. With the right configuration, we can all use the technology to save lives and help to protect vulnerable groups.”
Read more about keeping safe during lockdown:
- Coronavirus: Is hand-washing really the best thing we can do to stop the spread of COVID-19?
- Coronavirus: Should we all wear face masks?
The experts used a model city of one million people to simulate the impact of contact tracing software.The research suggested that as well as speed, a large number of users would also be needed to effectively slow the spread.
It indicates that if around 60 per cent of the whole population – and 80 per cent of those with a smartphone – used the software alongside other interventions it could stop the pandemic, but even a lower usage rate could at least slow the spread.
Professor Christophe Fraser, senior author of the Nuffield report, said: “Our results suggest a digital contact tracing app, if carefully implemented alongside other measures, has the potential to substantially reduce the number of new coronavirus cases, hospitalisations and ICU admissions.
“Our models show we can stop the epidemic if approximately 60 per cent of the population use the app, and even with lower numbers of app users, we still estimate a reduction in the number of coronavirus cases and deaths.”
According to a survey carried out by behavioural economists working with the Oxford University team, just over 73 per cent of people in the UK would be likely to install a contact tracing app for COVID-19.The experts added it is important any concerns about privacy and data usage are addressed at every stage of app development.
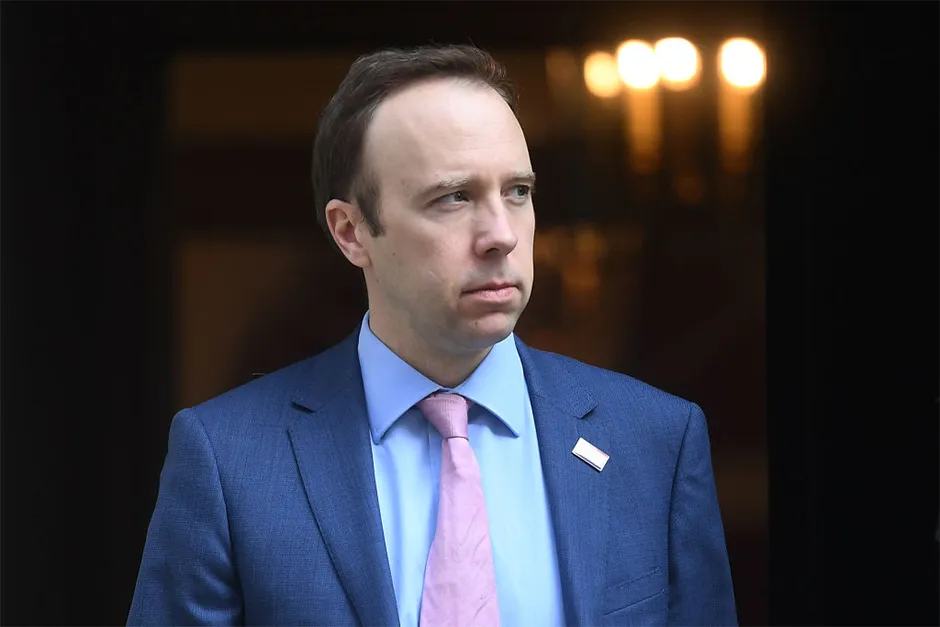
Health Secretary Matt Hancock has said developers of the NHS app are working with the world’s leading tech companies and experts in clinical safety and digital ethics “so that we can get this right”.
Prof Fraser said he hopes the new research would help push forward the development of an app.“We need strategies to exit from the lockdown whilst minimising the risk of resurgence,” he said.
“Combined with other interventions such as community testing and continued shielding of vulnerable individuals, digital contact tracing can help prevent coronavirus from rapidly re-emerging.
“We hope these latest findings will provide valuable evidence that mobile contact tracing can be carefully deployed after consideration of key epidemiological parameters, combined with critical ethical principles, to ensure we can save lives, reduce the number of people who need to remain in self-isolation, and support as many people as possible to safely and responsibly start returning to active life again.”
Read more about the coronavirus:
- Mental health impact of coronavirus outbreak ‘requires urgent study’
- Why are non-COVID related deaths on the rise?
A separate Policy Exchange report says a new cross-government and multi-agency testing and tracing command centre should be created to oversee the response to the crisis.
It says the centre would be led by a single individual with experience in command, control, coordination and communication and involve input from the NHS and other health authorities, the Government, police, military, intelligence agencies and the private sector.
Co-authored by Richard Walton, Policy Exchange senior fellow and former head of counter-terrorism command in the Metropolitan Police, the report also urges the Government to make a national appeal to the UK population to subscribe to the contact tracing app.
“The recent outbreak of COVID-19 has exposed the limitations of traditional manual contact tracing methods, a fact that leaders of some Asian economies – including South Korea and Singapore – had already understood after their handling of previous pandemics,” Mr Walton said.
“The UK will need to go much further in the use of new technology if it is to suppress further outbreaks of the disease. A testing and tracing command centre will be essential to this effort.”
Can I get the coronavirus twice?
There have been a few stories in the press of people apparently being re-infected by the coronavirus SARS-CoV-2. These people reportedly became infected and hospitalised, and then were sent home once they’d tested negative for the virus. Then, days or weeks later, they tested positive again.
But this doesn’t necessarily mean that they caught the coronavirus twice.
First, during recovery from infection, a person may have very low amounts of the virus remaining in their body – low enough that our tests can’t accurately detect it. In this case, the person may be sent home on the assumption that they’re virus-free. However, their body may still be fighting the virus, and a resurgence of the virus (and symptoms) can occur, resulting in a positive test. In this case, it would just be one protracted infection, not a re-infection.
Second, we know that in most people, SARS-CoV-2 generates a strong response from the immune system. With the related coronavirus SARS-CoV, this response creates an immune memory of the virus that prevents re-infection for one to two years, and it’s likely that this is also the case for the new virus. SARS-CoV-2 also has a fairly low mutation rate, which means that it (hopefully) won’t change enough that our immune system no longer remembers it (this is what the flu virus does and why we need a new jab every year).
If this all turns out to be true, then it would suggest that re-infections are unlikely and that the cases in the news reflect testing sensitivity. However, SARS-CoV-2 is so new that we won’t know for sure until we’ve found out just how protective our immune response to the virus is, and how long it lasts.
Read more: